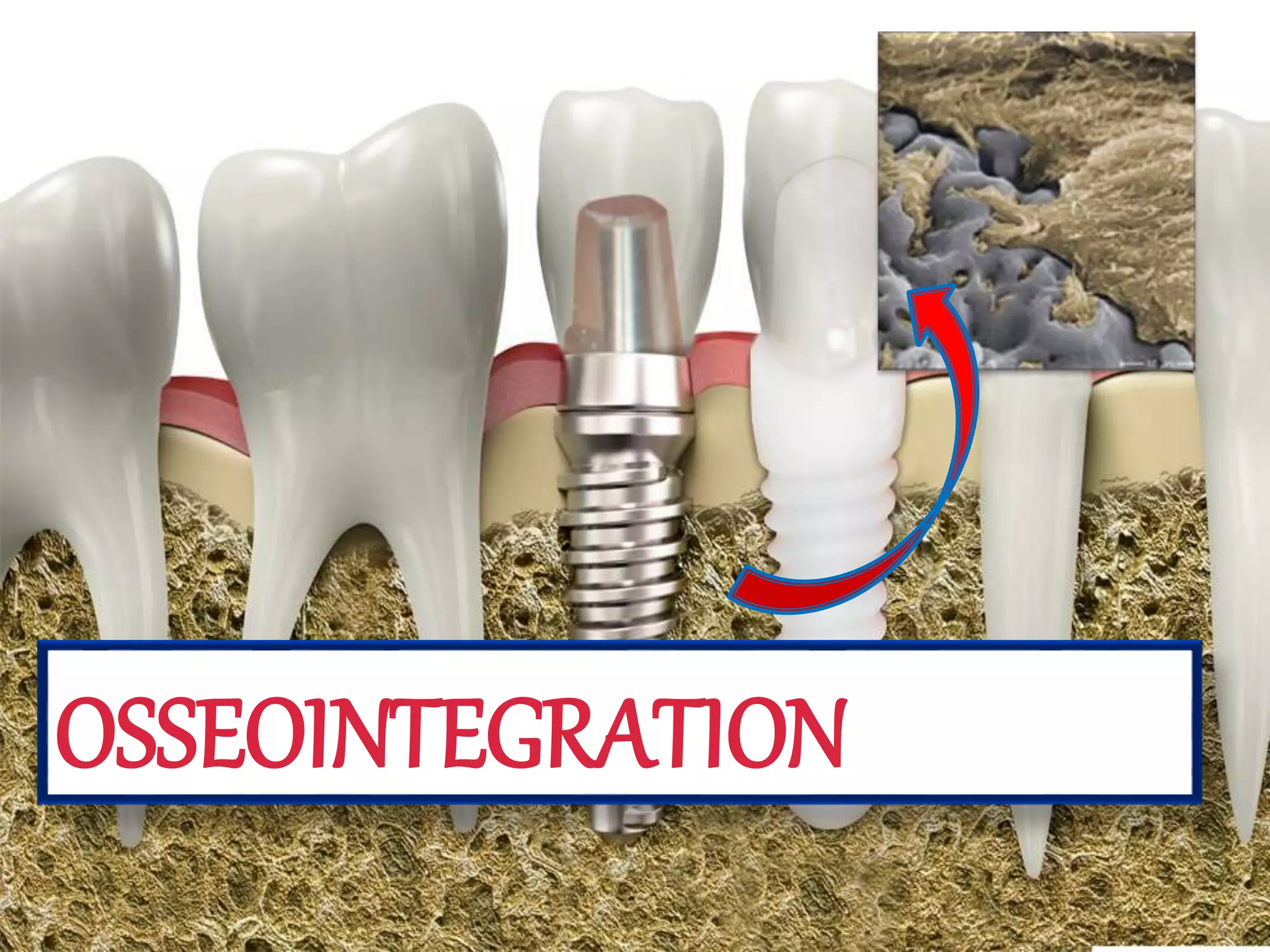
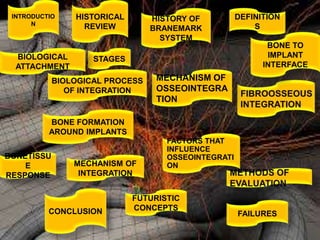
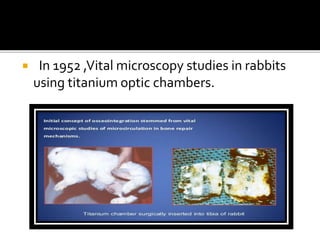
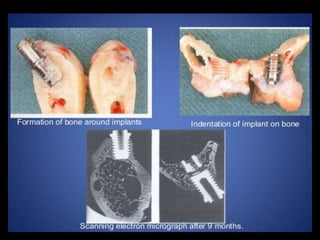
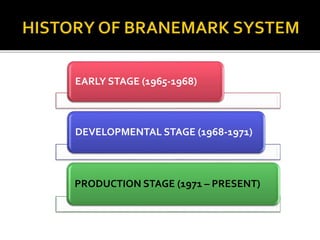
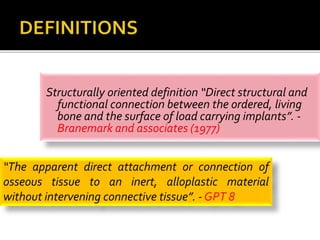
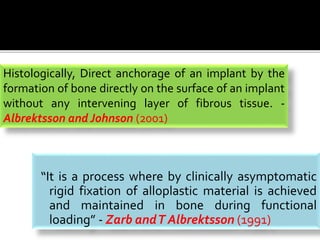
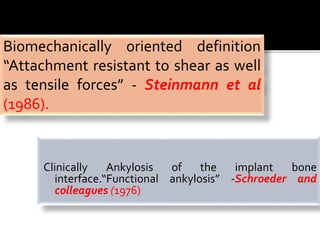
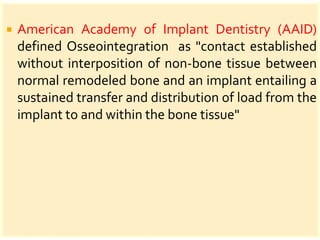
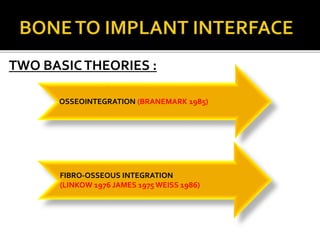
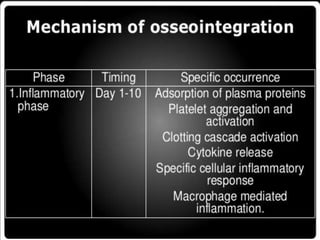
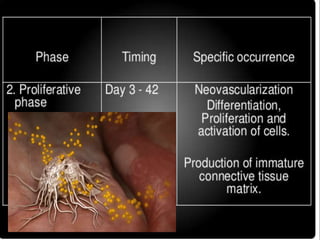
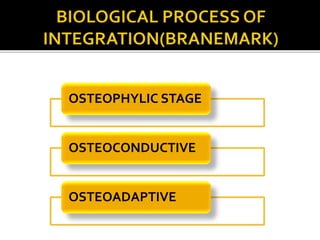
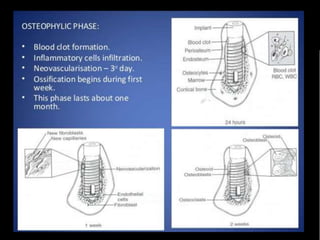
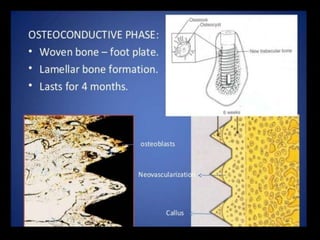
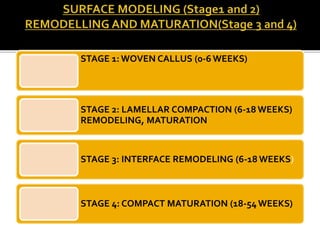
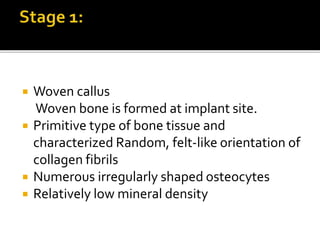
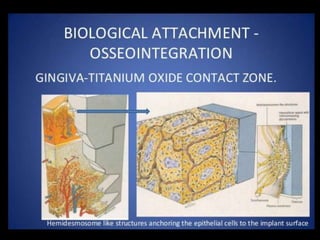
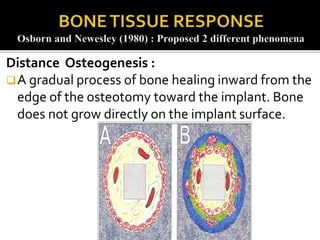
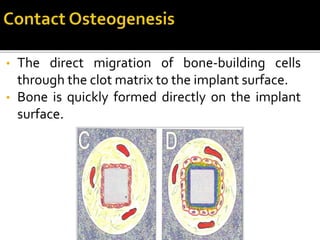
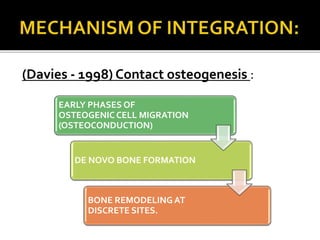
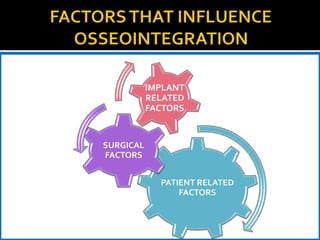
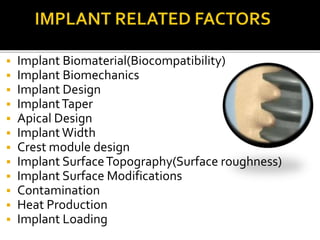
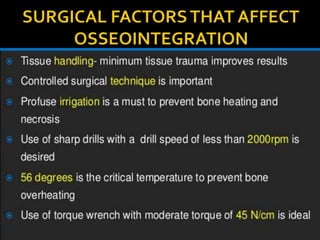
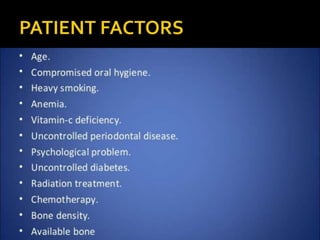
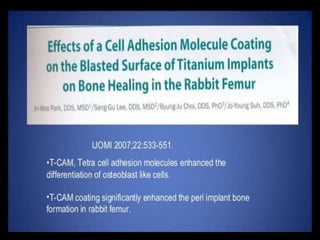
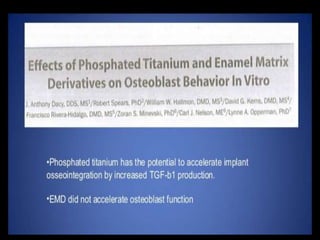
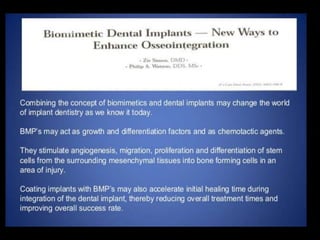
This document discusses osseointegration, which refers to the direct structural and functional connection between bone and the surface of a load-bearing dental implant without intervening soft tissue. It traces the history and development of osseointegration from early experiments in the 1950s to its current understanding. The key aspects covered include definitions of osseointegration, the biological process of bone formation around implants over time, factors that influence osseointegration success, and future directions for improving integration.