This document provides information on temporomandibular disorders (TMD) including:
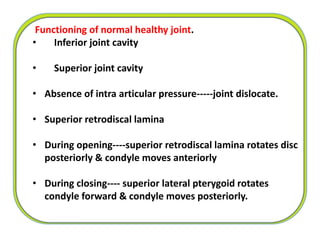
- TMD is defined as abnormal, incomplete, or impaired function of the temporomandibular joint and muscles of mastication.
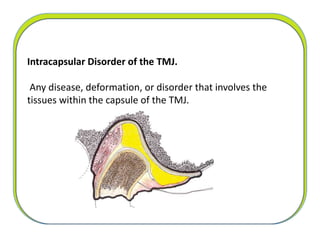
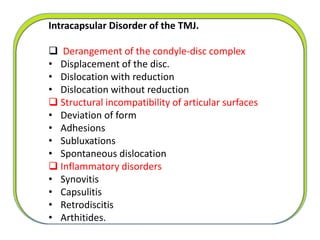
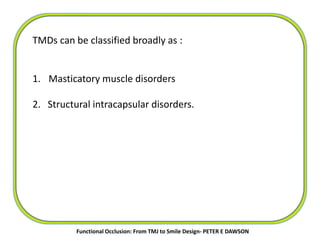
- TMDs can be classified as masticatory muscle disorders, structural intracapsular disorders, or conditions that mimic TMD.
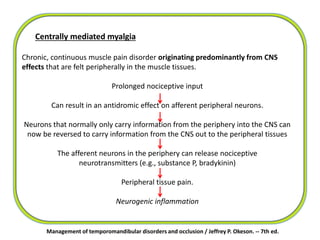
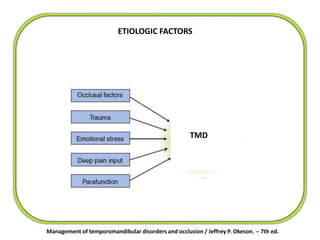
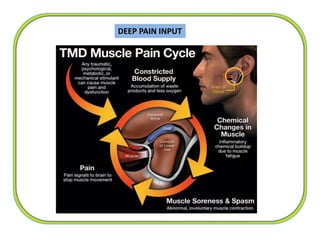
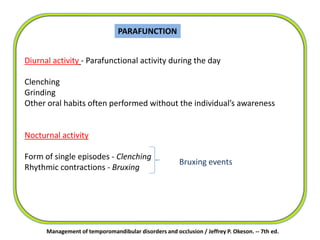
- Etiological factors of TMD include occlusal factors, trauma, emotional stress, parafunction such as clenching or bruxism, and deep pain input. Protective muscle co-contraction, local muscle soreness, myofascial pain, and centrally mediated myalgia are some masticatory muscle disorders discussed.
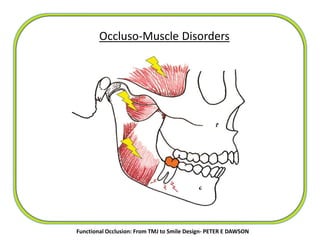
![More specific classification [PETER E DAWSON ]
Category 1: Occluso-muscle disorders with no intracapsular defects.
Category 2 :Intracapsular disorders that are directly related to occlusal
disharmony and are reversible in re-establishing comfortable function
if the occlusion is corrected.
Category 3 :Intracapsular disorders that are not reversible, but because
of adaptive changes, can function comfortably if occluso-muscle
harmony is re-established.
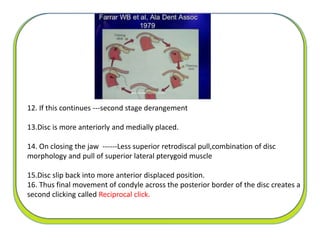
Category 4 :Nonadapted intracapsular disorders that may be either
primary or secondary to occlusal disharmony or may be unrelated.
Functional Occlusion: From TMJ to Smile Design- PETER E DAWSON](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-18-320.jpg)
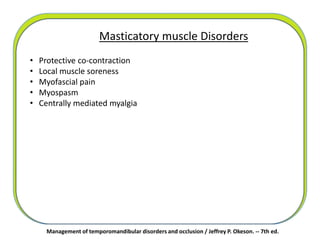
![Masticatory muscle disorders
Temporomandibular joint
(TMJ) disorders
Chronic mandibular hypomobility
Growth disorders
• Protective co-contraction
• Local muscle soreness
• Myofascial pain
• Myospasm
• Centrally mediated myalgia
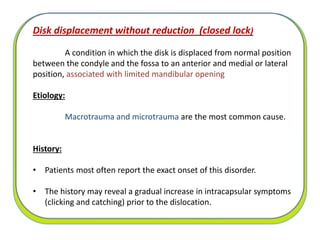
• Derangement of the condyle-disc complex
• Structural incompatibility of the articular surfaces
• Inflammatory disorders of the TMJ
• Ankylosis
• Muscle contracture
• Coronoid impedance
• Congenital and developmental bone disorders
• Congenital and developmental muscle disorders
Classification System for Diagnosing Temporomandibular Disorders
[ OKESON JP ]
Management of temporomandibular disorders and occlusion / Jeffrey P. Okeson. -- 7th ed.](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-19-320.jpg)
![CLASSIFICATION
[American Academy of Orofacial Pain] – McNeil
Articular
•Developmental
Deviation of form.
•Disc displacement
With reduction.
Without reduction.
•Hypermobility.
•Dislocation.
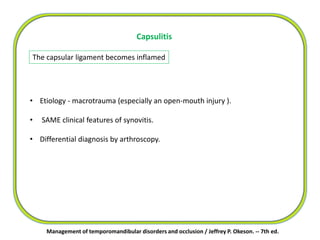
•Inflammatory
Synovitis.
Capsulitis.
•Arthritides
Osteoarthrosis.
Osteoarthritis.
Polyarthritides.
•Ankylosis
Fibrous / bony
Non-Articular OR Masticatory muscle disorders.
•Myofascial pain.
•Myositis.
•Spasm.
•Protective splinting.
•Contracture.
•Neoplasia.
McNeill Charles : Management of temporomandibular disorders. J Prosthet Dent 1997; 77: 510-22.](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-20-320.jpg)
![TRAUMA
Greater impact on intracapsular disorders than on muscular disorders.
Macrotrauma [ eg :-Direct blow to the face ]
Trauma
Microtrauma. [ eg :-Clenching, Bruxism ]
Management of temporomandibular disorders and occlusion / Jeffrey P. Okeson. -- 7th ed.](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-27-320.jpg)
![Management of temporomandibular disorders and occlusion / Jeffrey P. Okeson. -- 7th ed.
Stress affects the body by activating the
hypothalamic-pituitary-adrenal (HPA) axis
The HPA axis
[ through complex neural pathways]
Increases the activity of the gamma efferents
Intrafusal fibers of the muscle spindles to contract
sensitized spindles
Any slight stretching of the muscle will cause a
reflex contraction
Increase in the muscle’s tonicity.
EMOTIONAL STRESS](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-28-320.jpg)
![Protective co-contraction [ protective muscle splinting ]
Deep pain input or an increase in emotional stress
Sudden change in sensory or proprioceptive input from associated
structures
CNS response to injury or threat of injury
First response of the masticatory muscles
Management of temporomandibular disorders and occlusion / Jeffrey P. Okeson. -- 7th ed.
Key to identify Protective splinting immediately follows an event
If continues for several hours or days, the muscle tissue can
become compromised and a local muscle problem may develop](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-34-320.jpg)
![Management of temporomandibular disorders and occlusion / Jeffrey P. Okeson. -- 7th ed.
Myofascial pain ( Trigger point myalgia)
Deep pain input
+
Increased levels of emotional stress
[ upregulation of the autonomic nervous system ]
excite peripheral sensory neurons
(primary afferents)
antidromic release of algogenic substances into the peripheral tissues
(neurogenic inflammation)
muscle pain](https://image.slidesharecdn.com/sharitmdfirstpart-210908104605/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-first-part-37-320.jpg)