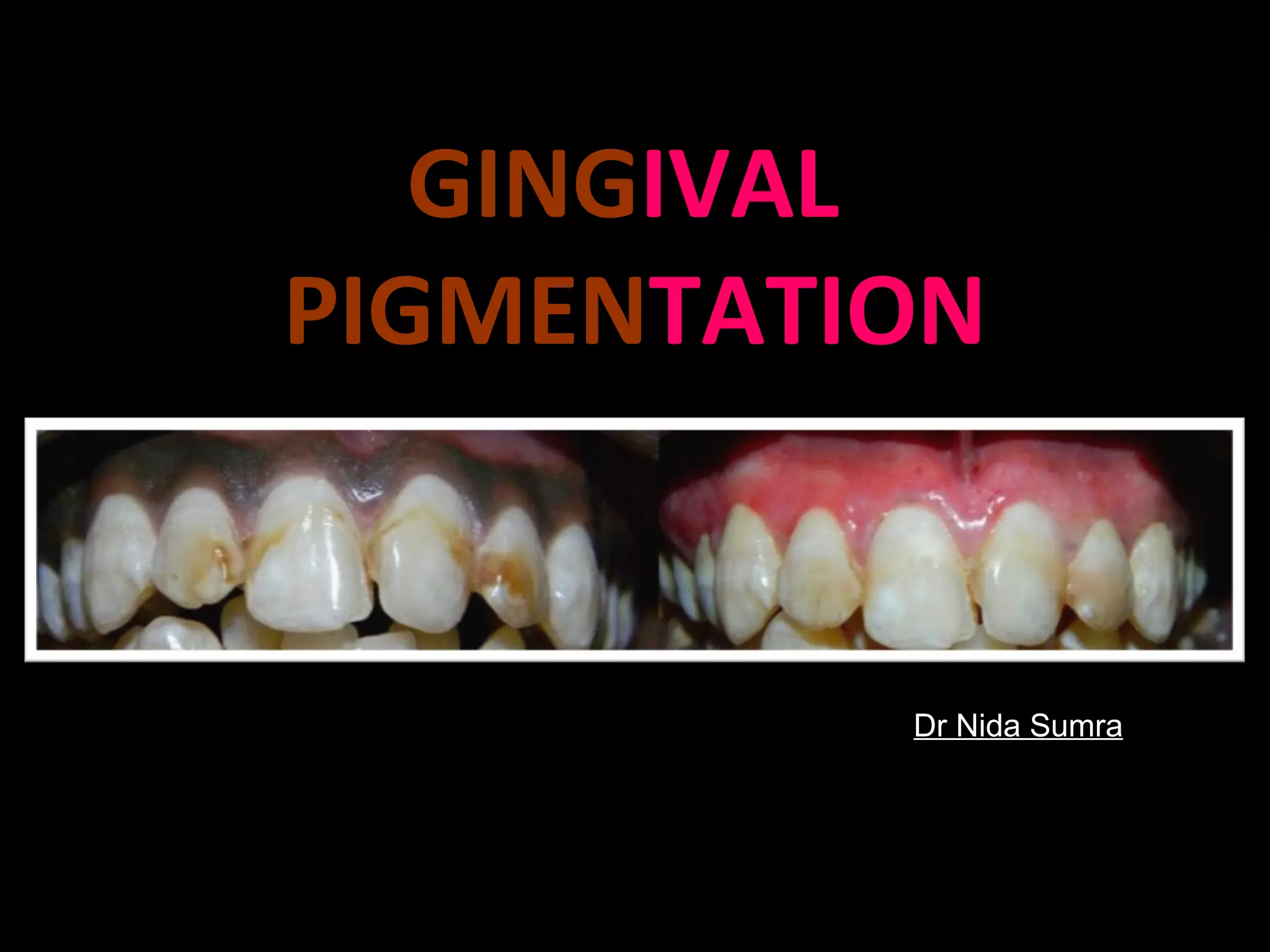
This document discusses gingival pigmentation from a historical, physiological, and clinical perspective. It begins by covering the historical descriptions of pigmentation in various populations dating back to the early 1900s. It then describes the structure and function of melanocytes and melanin, as well as the genetic, hormonal, and environmental factors that regulate melanin synthesis. The document classifies different types of pigmentation and pigmented lesions that can occur in the oral mucosa. Finally, it reviews various surgical and non-surgical methods that can be used to depigmentate abnormal gingival pigmentation.