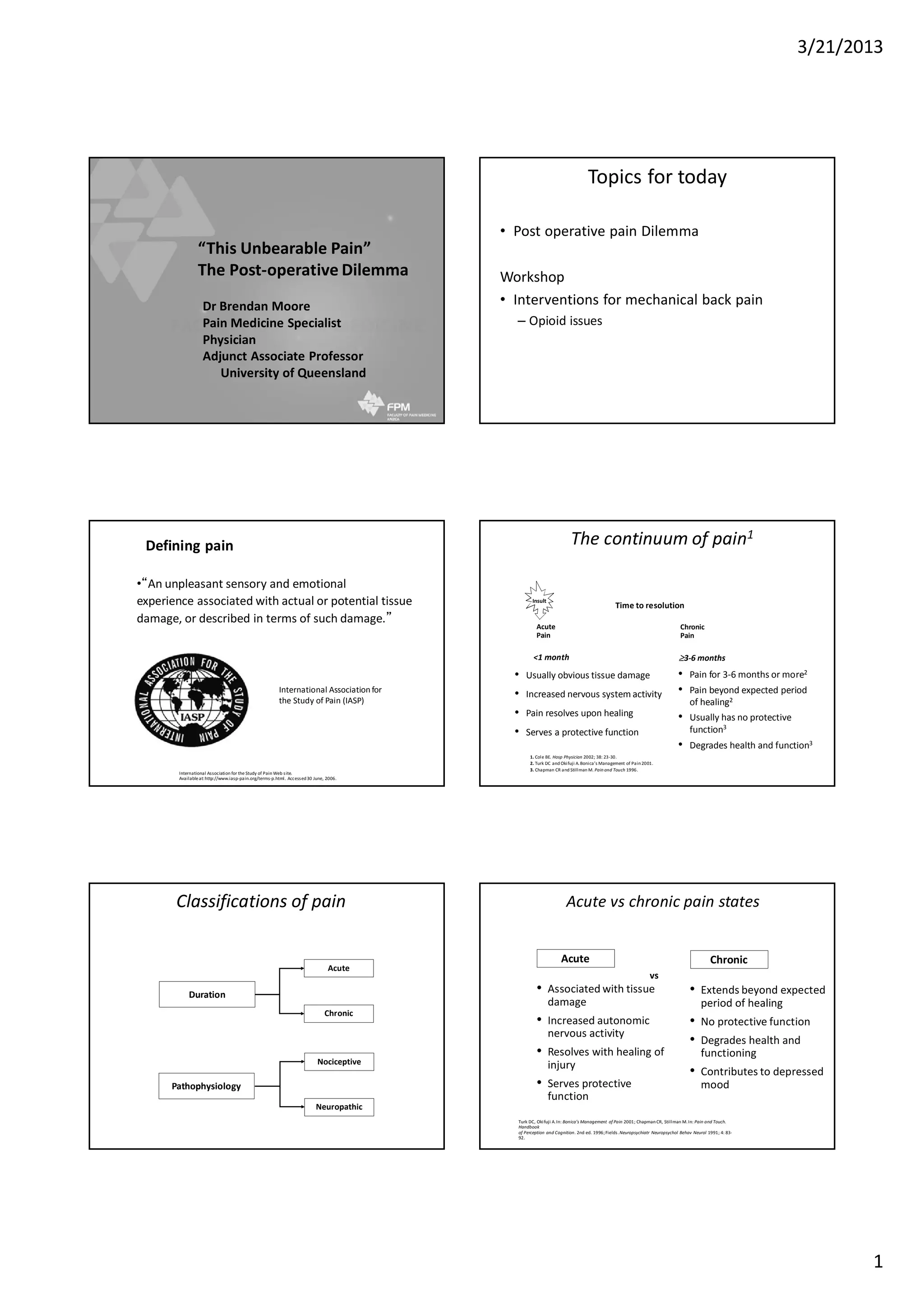
The document discusses post-operative pain management, distinguishing between acute and chronic pain, and various pain states including nociceptive and neuropathic pain. It emphasizes the importance of a comprehensive management plan that includes medication, physical rehabilitation, and understanding psychosocial factors affecting recovery. The document also highlights the role of healthcare providers in educating patients and coordinating care to improve outcomes and reduce the transition to persistent pain.