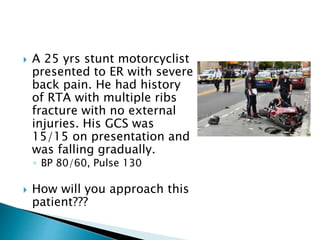
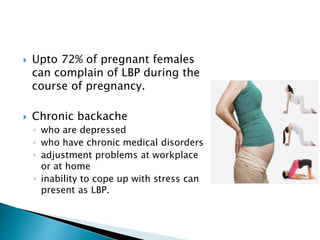
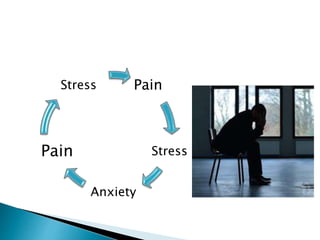
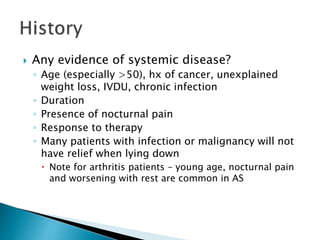
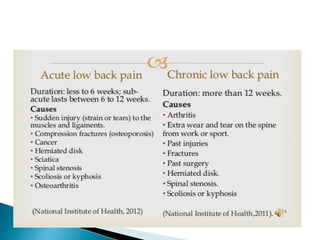
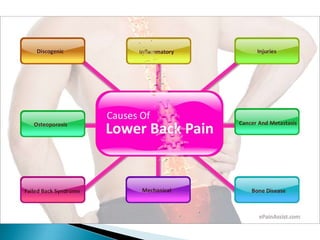
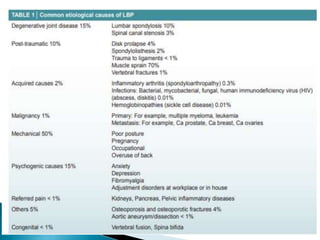
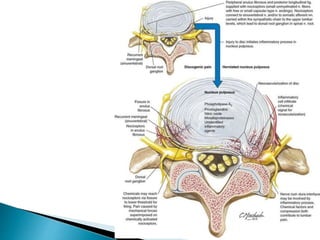
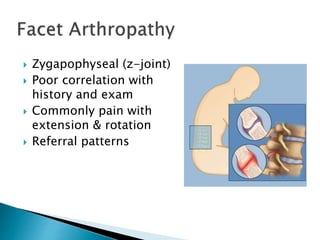
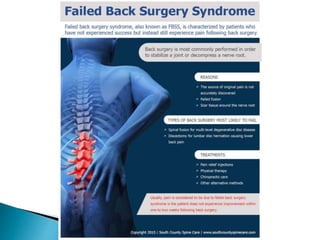
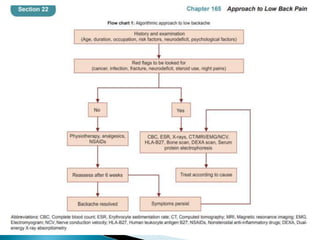
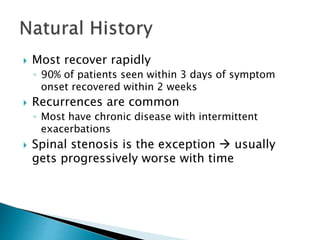
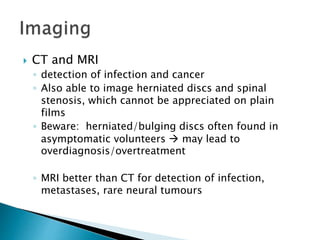
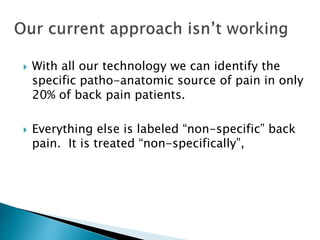
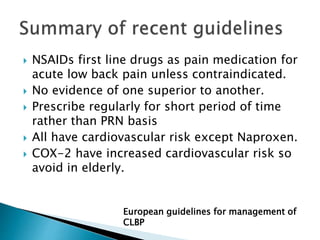
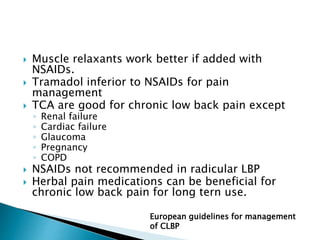
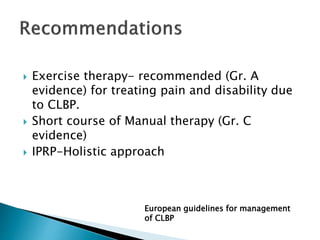
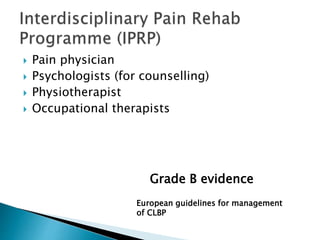
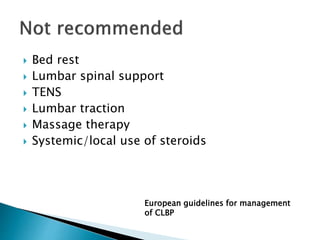
The document discusses several cases of patients presenting with low back pain and how to approach them. It provides guidance on red flags to watch out for that could indicate a serious underlying cause. Conservative treatment is generally recommended as the first approach unless red flags are present. This includes medications, physical therapy, exercise and counseling. Further investigation may be needed if red flags are present or the patient does not improve with initial treatment.