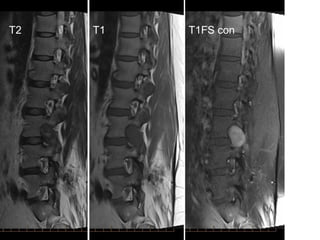
This document discusses several issues related to spine imaging. It covers the importance of radiation exposure from various imaging modalities like CT and highlights strategies to reduce radiation dose. Guidelines for imaging low back pain recommend no imaging for non-specific back pain but imaging if neurological deficits are present or specific causes are suspected. The document reviews imaging modalities like X-ray, bone scan, CT and MRI and what each shows. It provides details on MRI sequences and appearances of common spine findings.