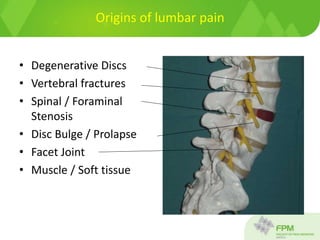
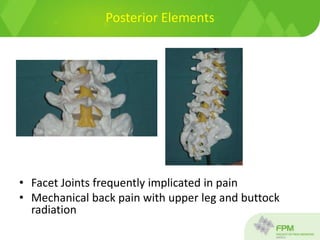
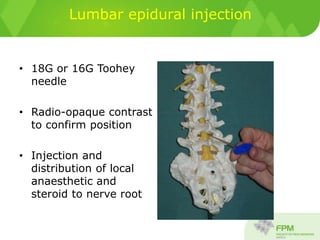
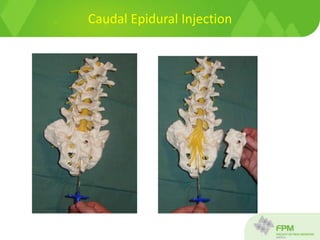
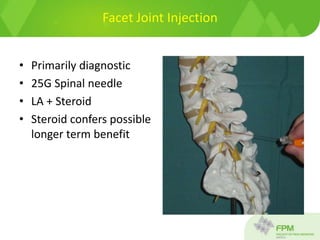
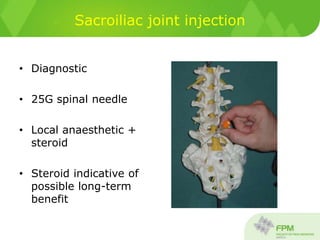
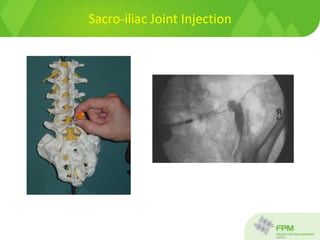
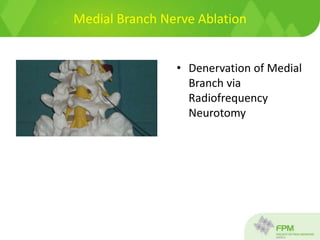
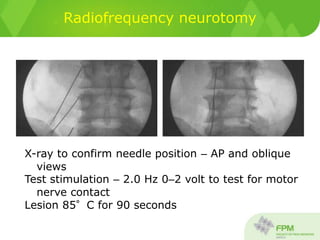
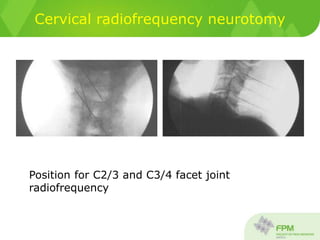
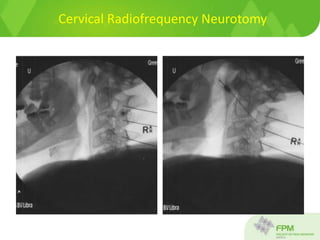
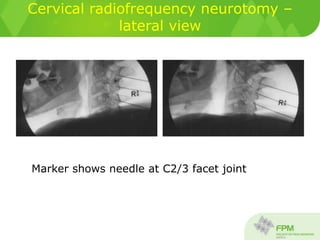
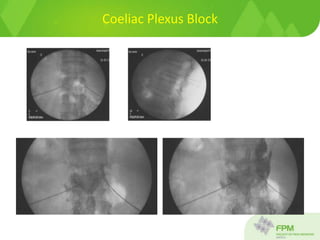
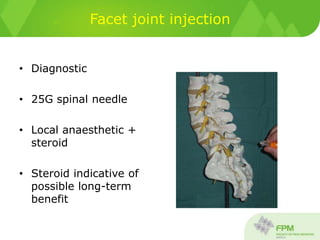
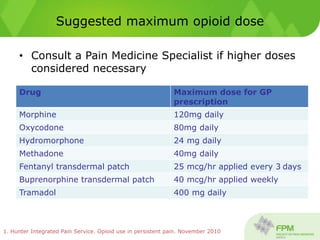
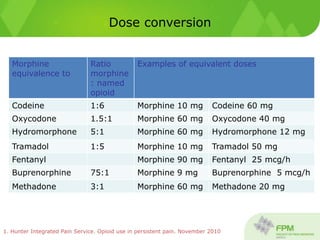
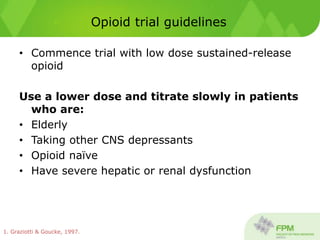
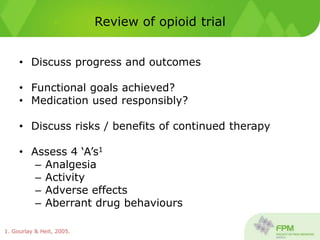
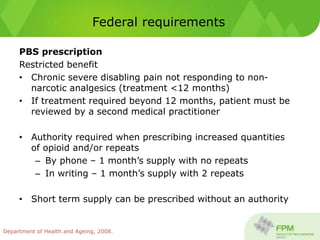
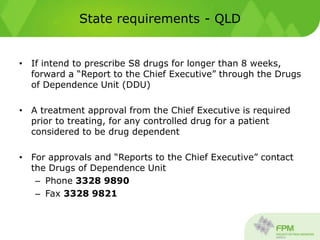
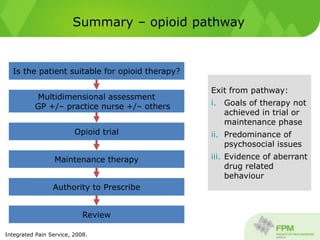
This document discusses interventional pain procedures for chronic pain, including epidural injections, facet joint injections, medial branch blocks, and radiofrequency nerve ablation. It provides details on how each procedure is performed, when they are appropriate, and their potential benefits which include temporary pain relief and allowing patients to progress in rehabilitation. It also covers guidelines for opioid prescribing for chronic pain, including maximum recommended doses, conversion between opioid medications, requirements for authorities to prescribe, and factors to consider in opioid trials and maintenance therapy.