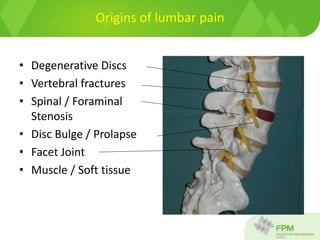
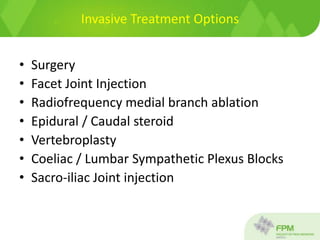
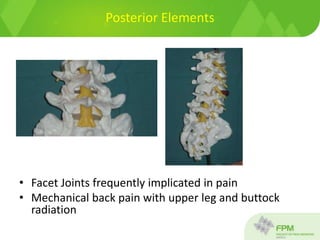
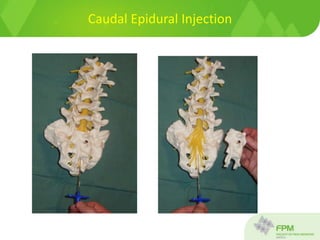
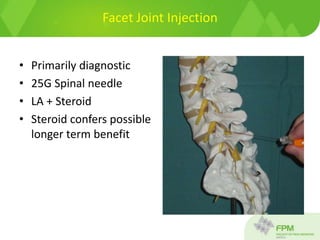
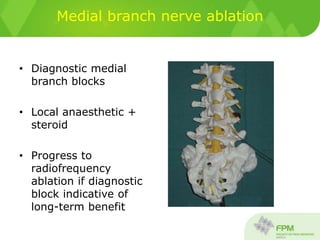
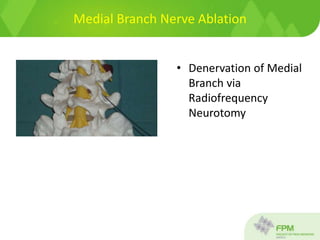
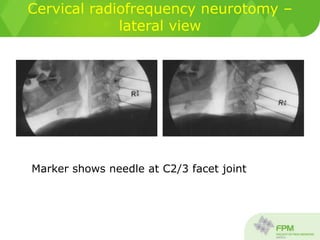
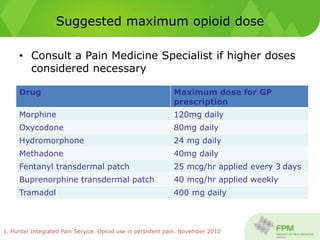
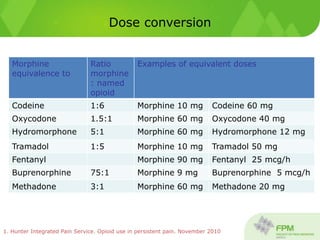
This document discusses interventional procedures for chronic pain, specifically in the lumbar back region. It describes common origins of lumbar pain such as degenerative discs and stenosis. Invasive treatment options are then outlined, including various injection procedures like epidural, facet joint, and medial branch nerve ablation using radiofrequency. The document provides details on how these procedures are performed and their goals in potentially providing temporary pain relief and allowing rehabilitation. Maximum recommended opioid doses and conversions between opioids are also presented.