1) Ultrasound uses high frequency sound waves to produce images of structures inside the body. It was introduced in the 1950s and has improved medical diagnosis. It is now also used in dentistry.
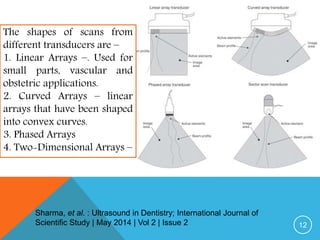
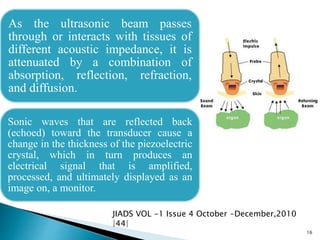
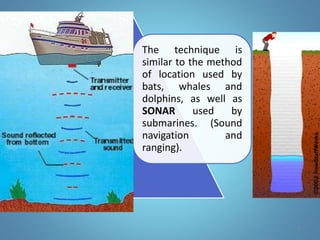
2) Ultrasound works by transmitting sound waves into the body via a transducer. Echoes from tissue interfaces are detected and displayed as images. Different transducer shapes produce different image scans for small parts, vascular, and obstetric applications.
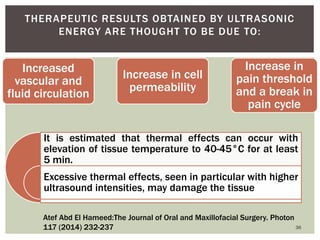
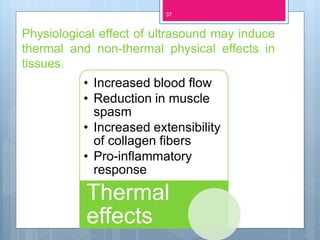
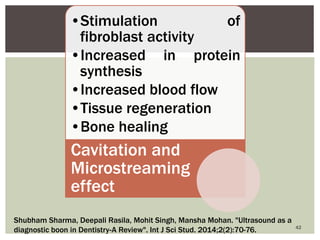
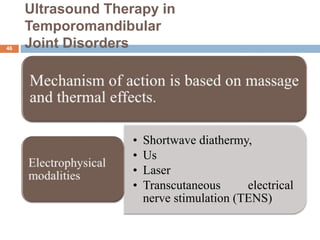
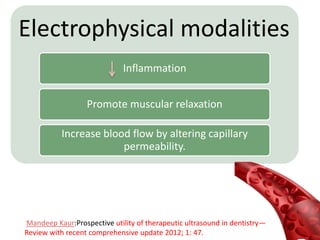
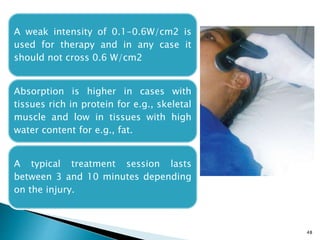
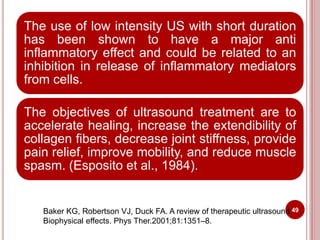
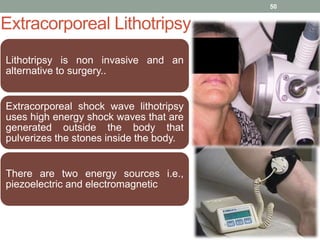
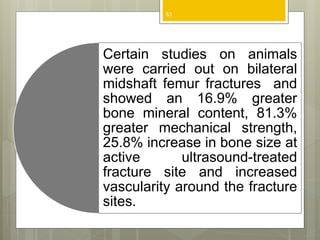
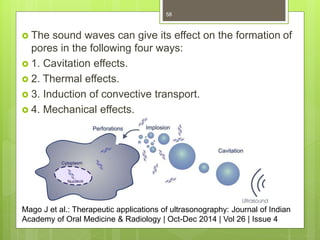
3) Therapeutic ultrasound uses lower intensities to increase blood flow, reduce muscle spasm, and accelerate healing. It has applications in temporomandibular joint disorders, bone healing, extracorporeal lithotripsy, and accelerating wound repair

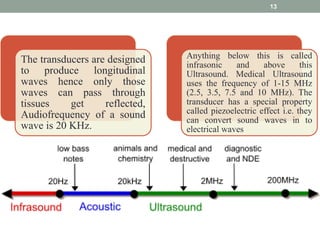
![The phenomenon perceived as sound is the
result of periodic changes in the pressure of air
against the eardrum.
The periodicity of these changes lies anywhere
between 1500 and 20,000 cycles per second
([Hz]).
By definition, ultrasound has a periodicity greater
than 20 kHz.
Diagnostic ultrasonography (sonography), the
clinical application of ultrasound, uses vibratory
frequencies in the range of 1 to 20 MHz.
9](https://image.slidesharecdn.com/jcultrasound-160426150204/85/ultrasound-in-dentistry-8-320.jpg)