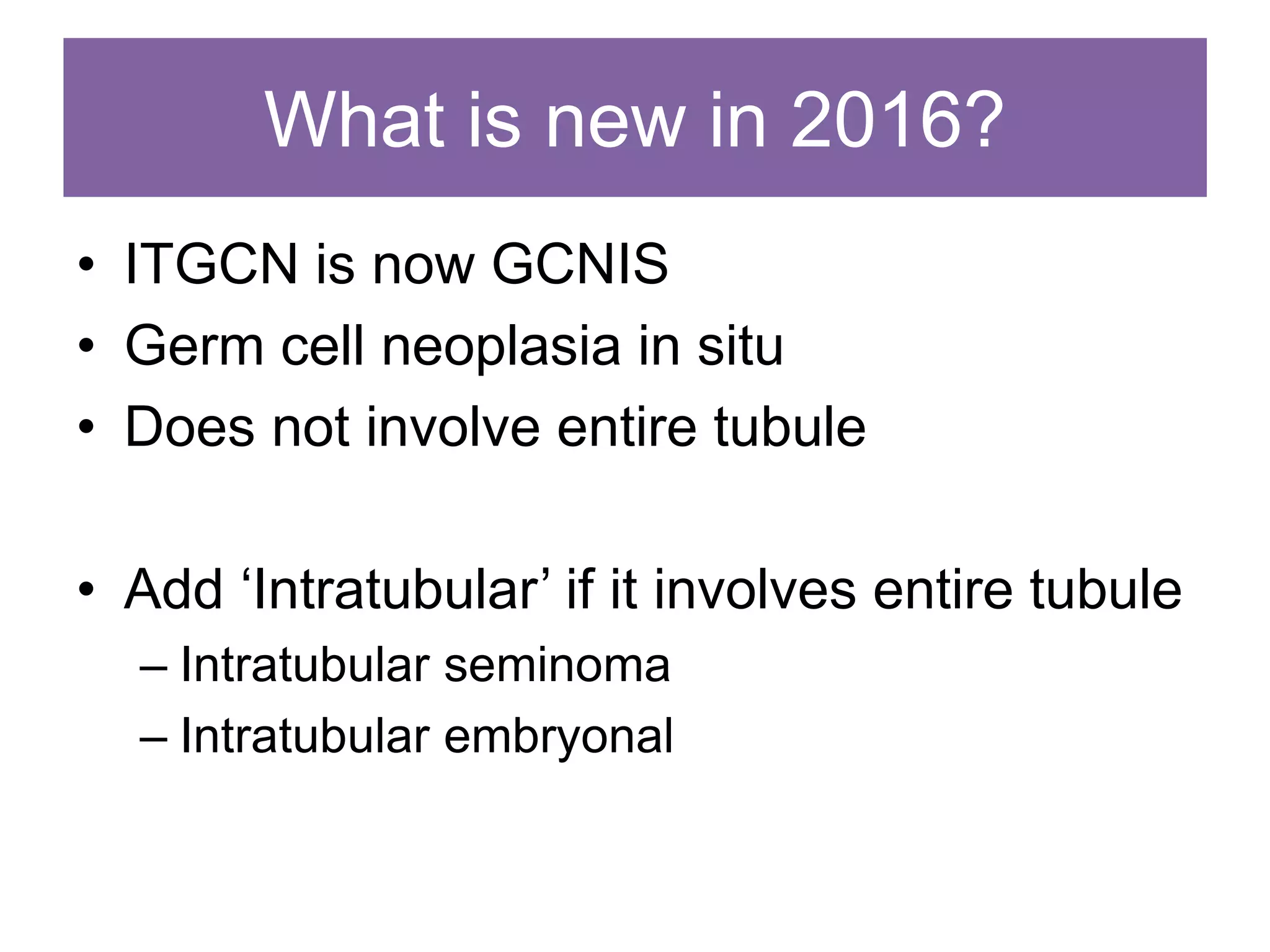
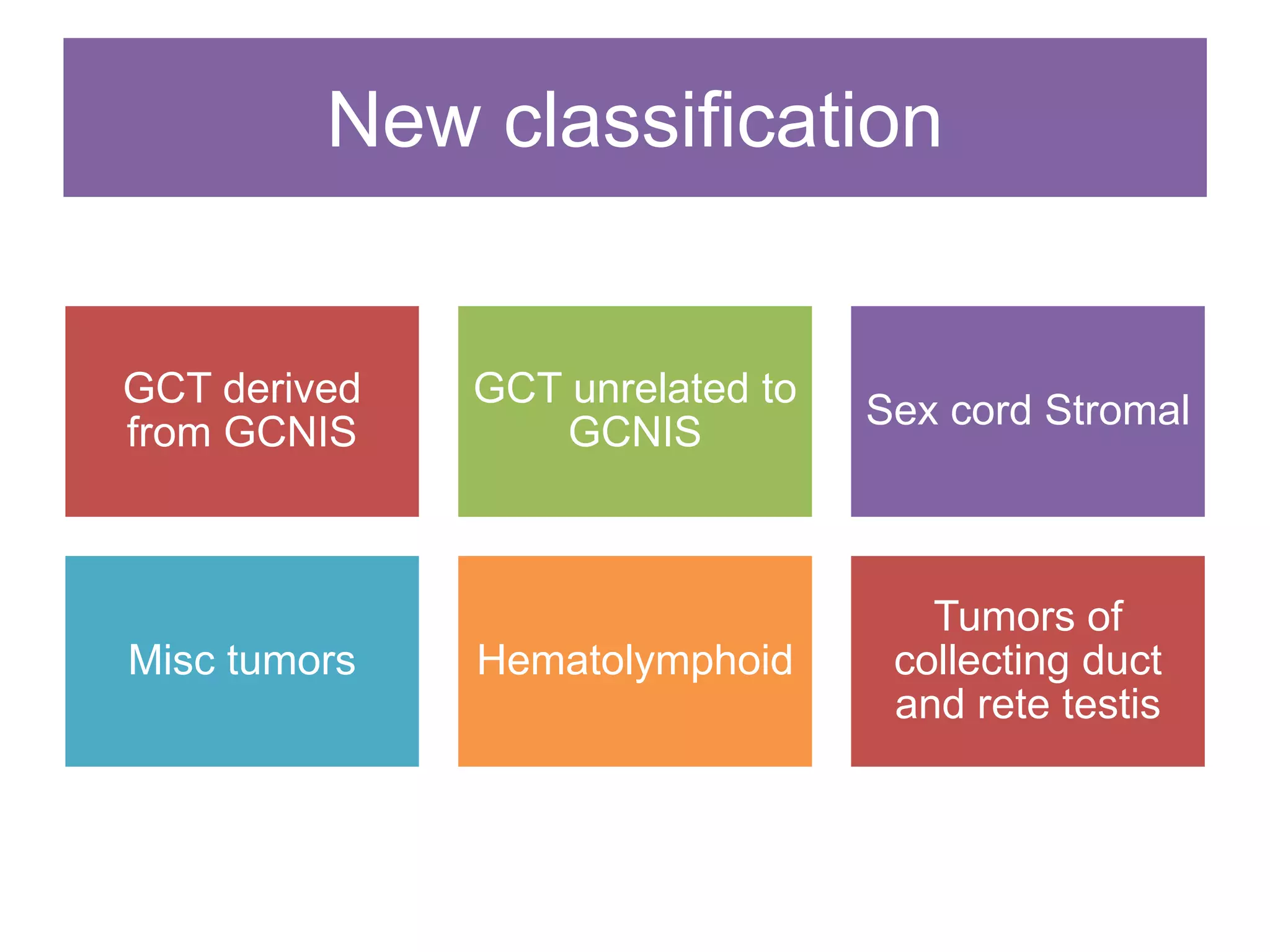
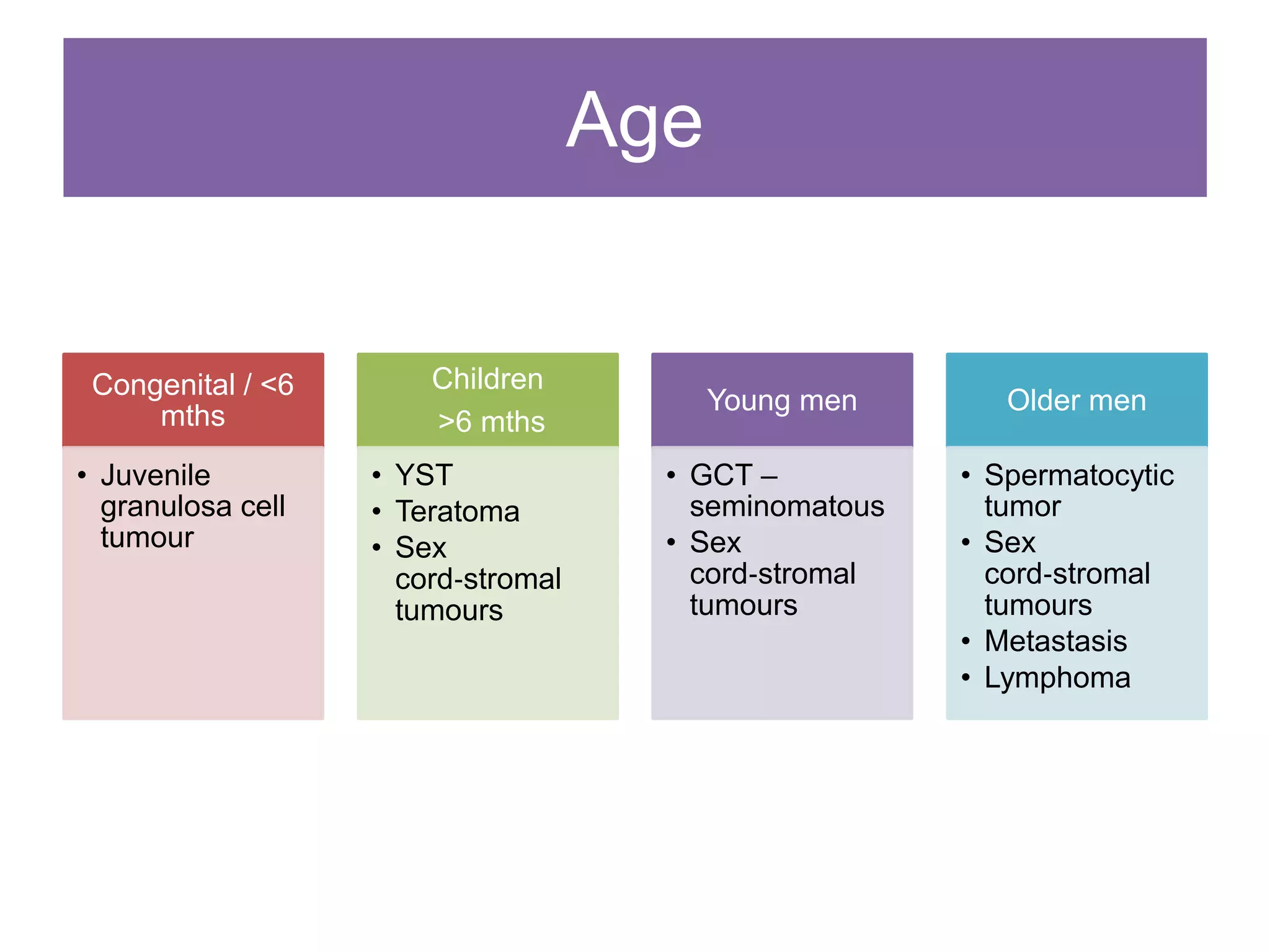
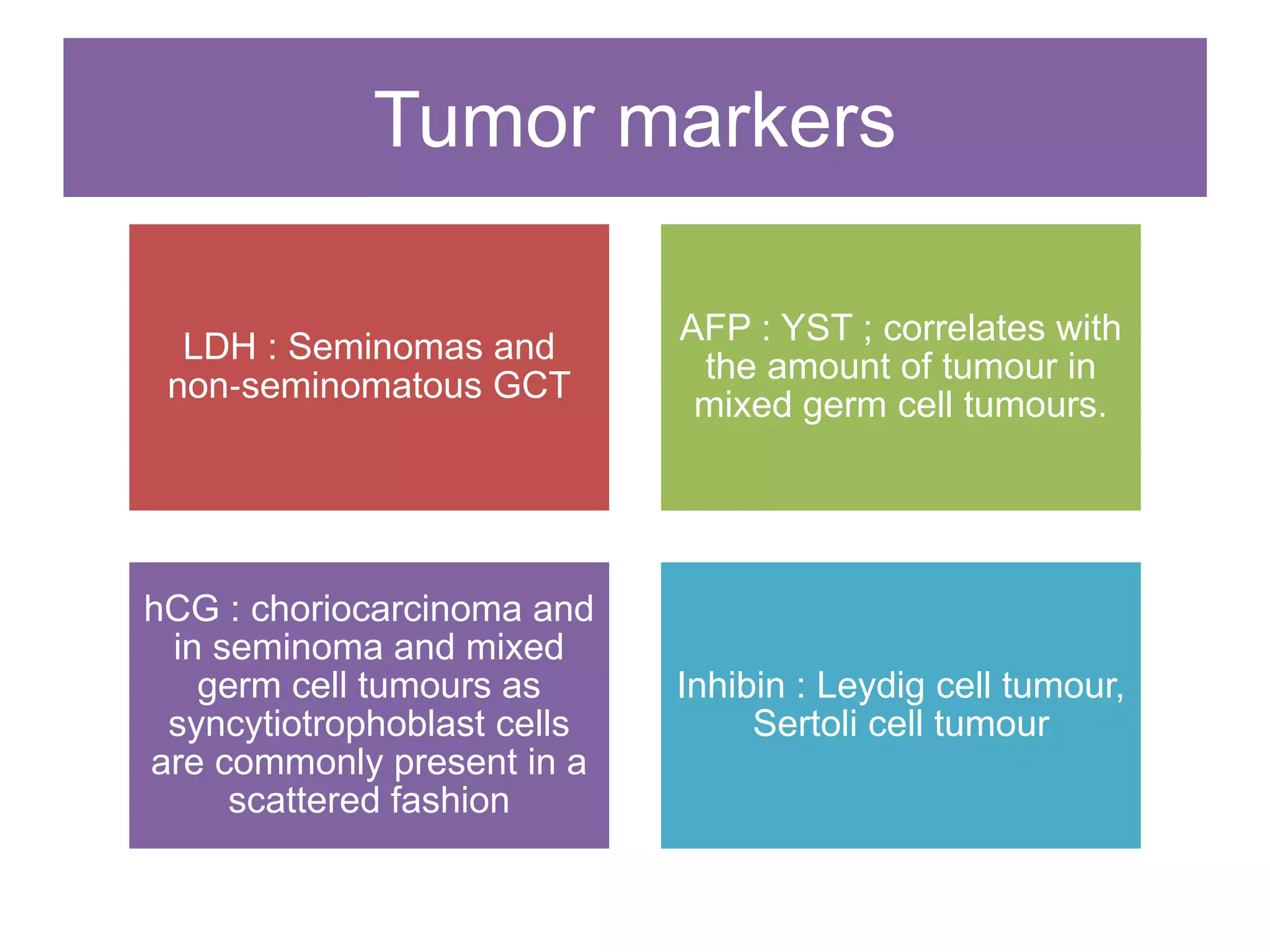
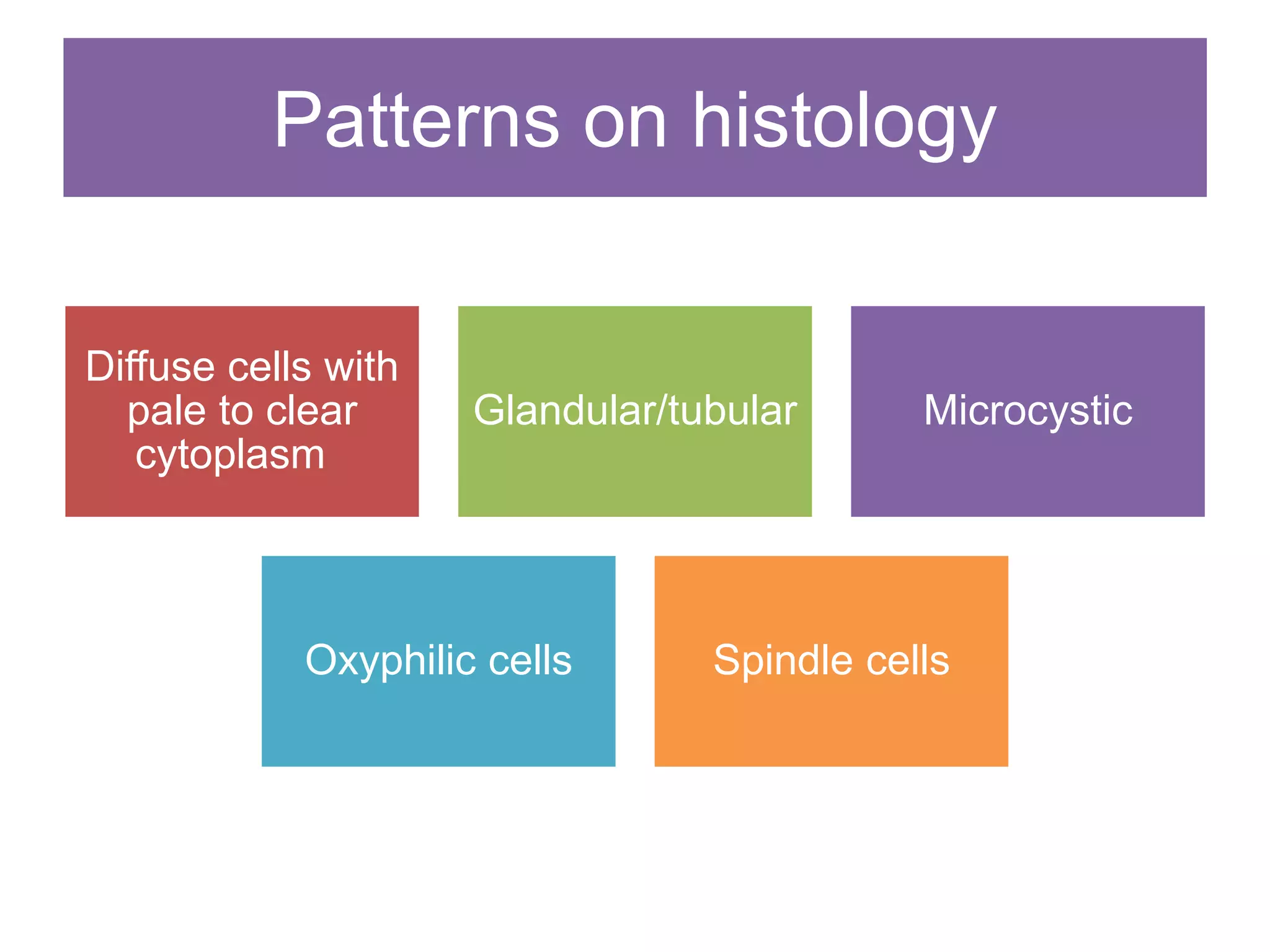
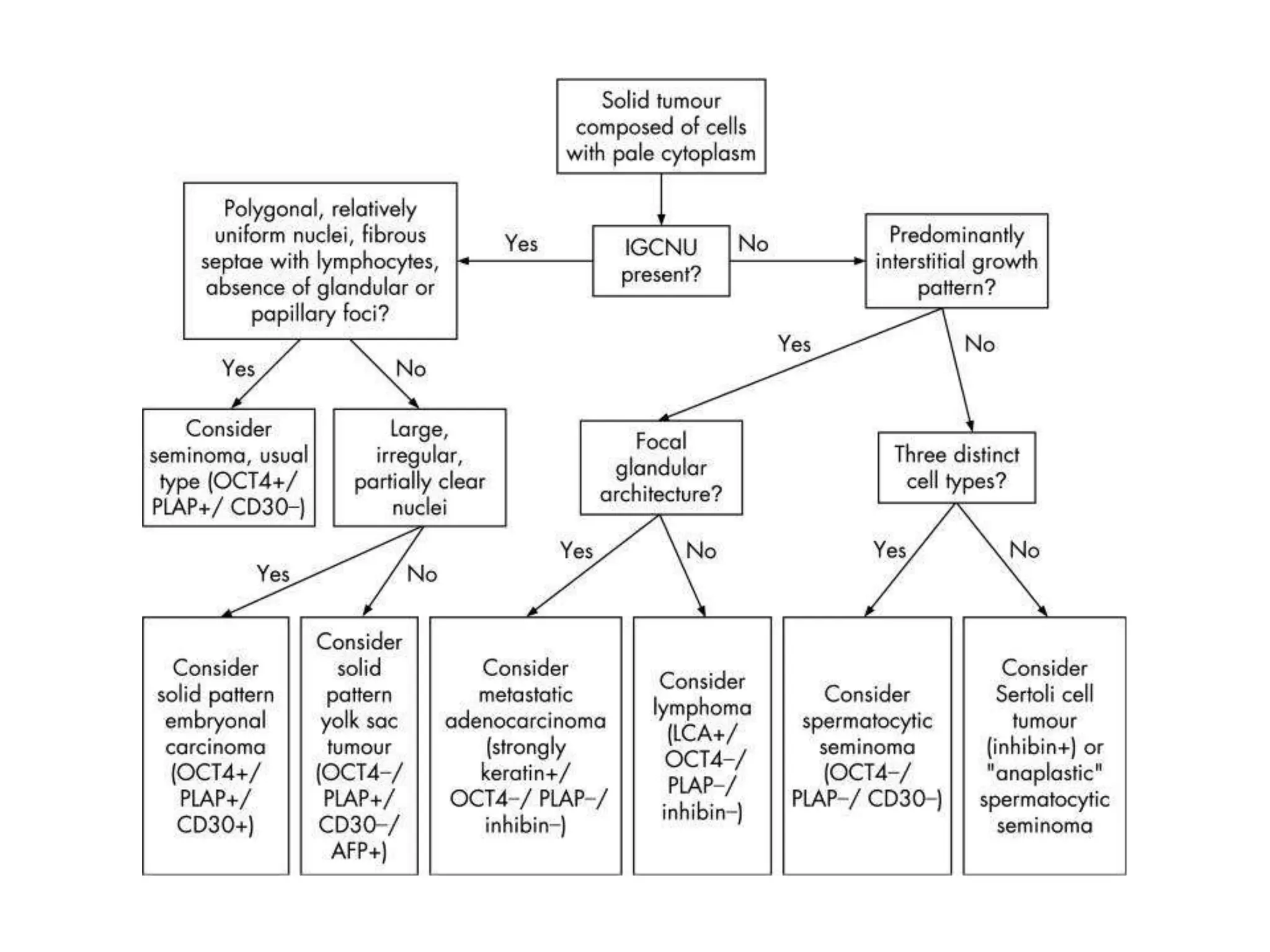
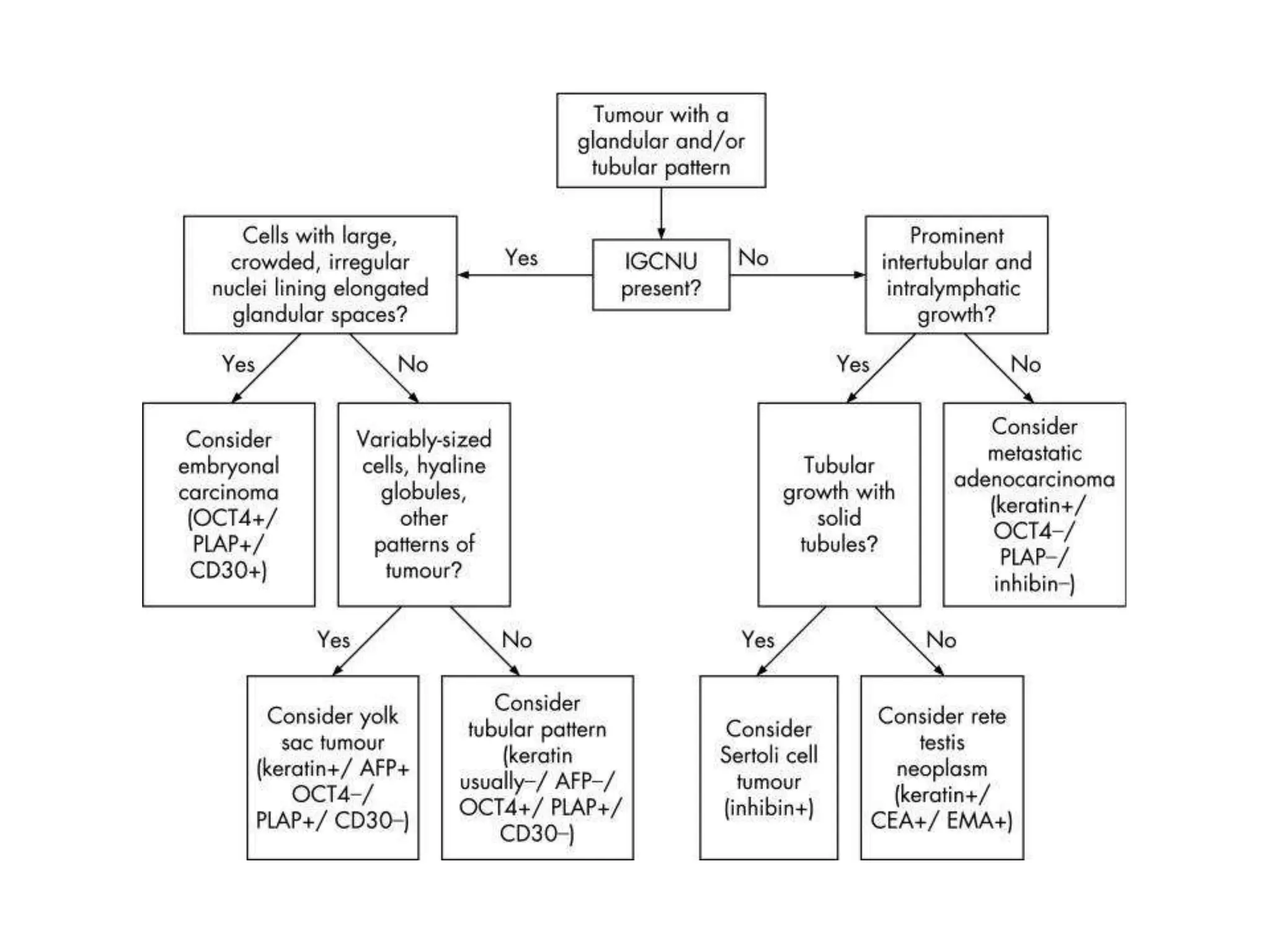
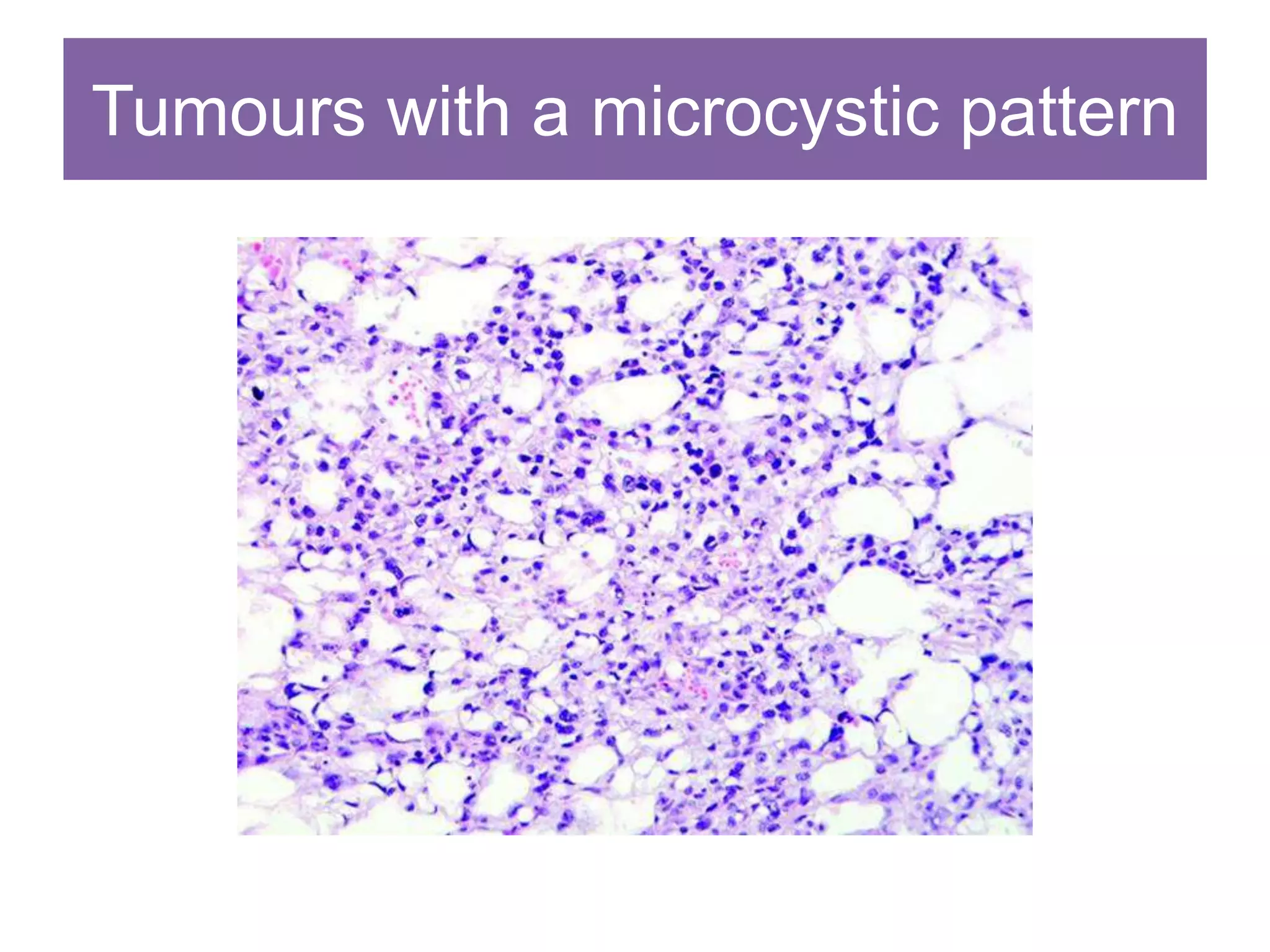
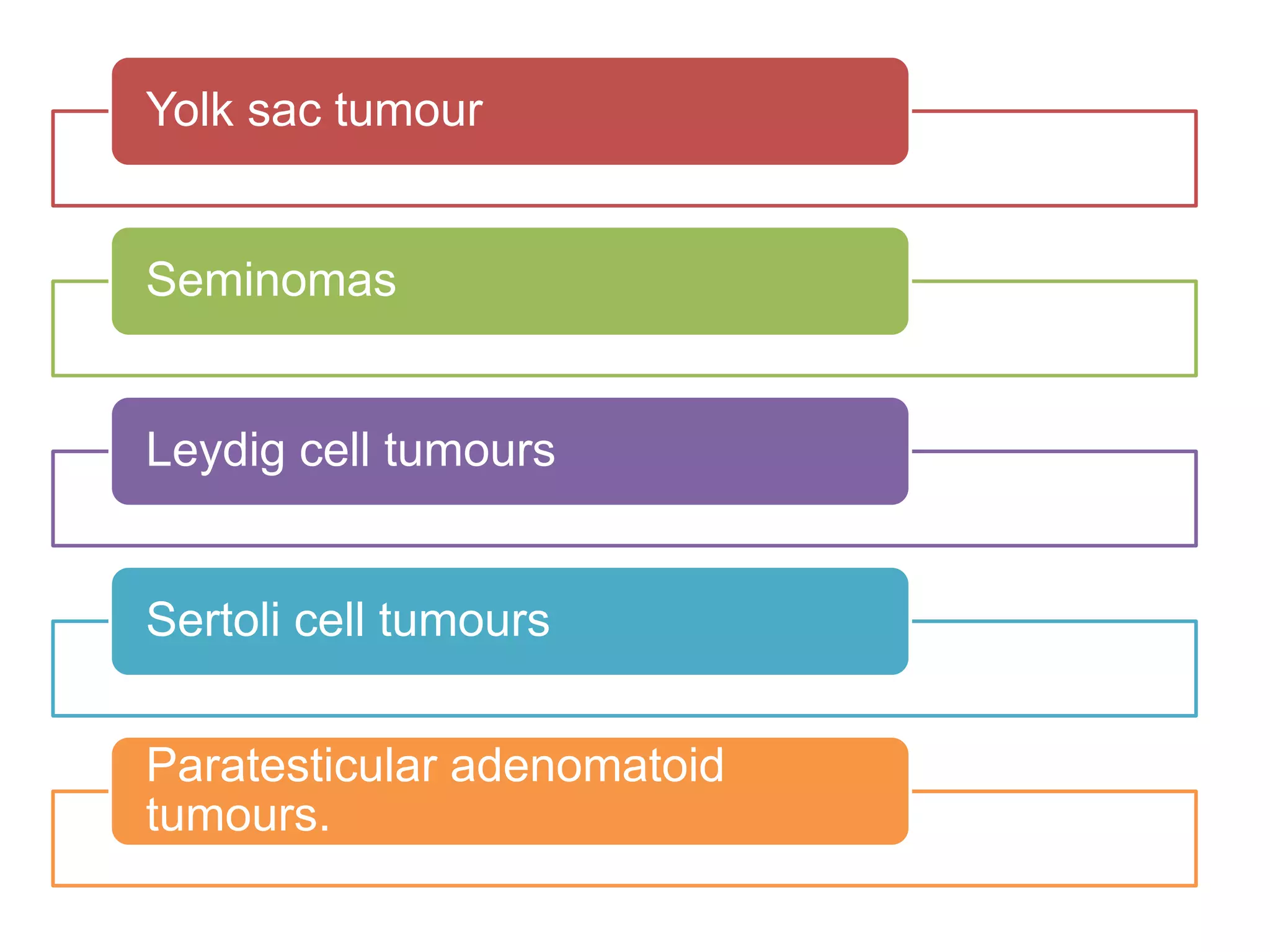
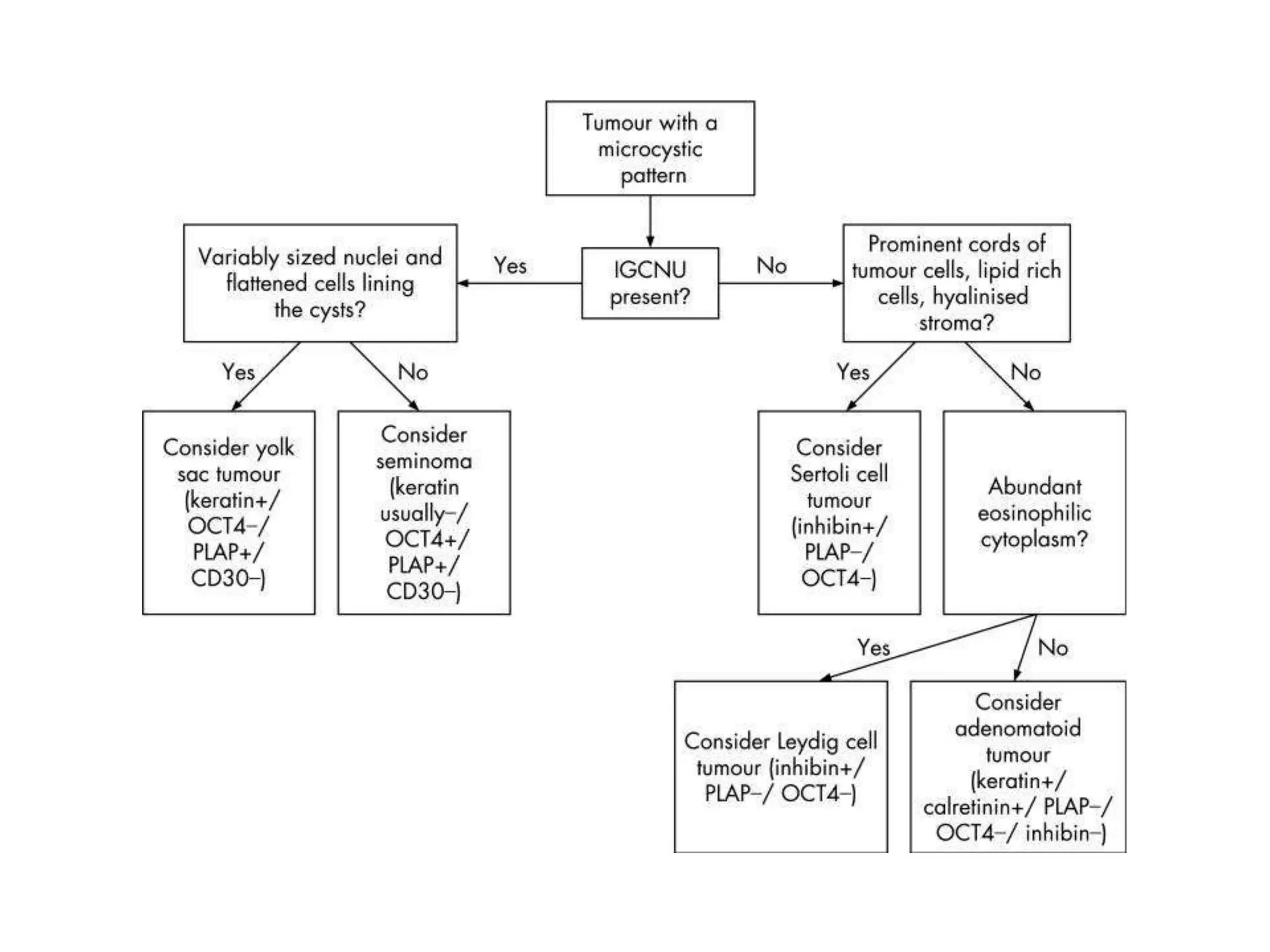
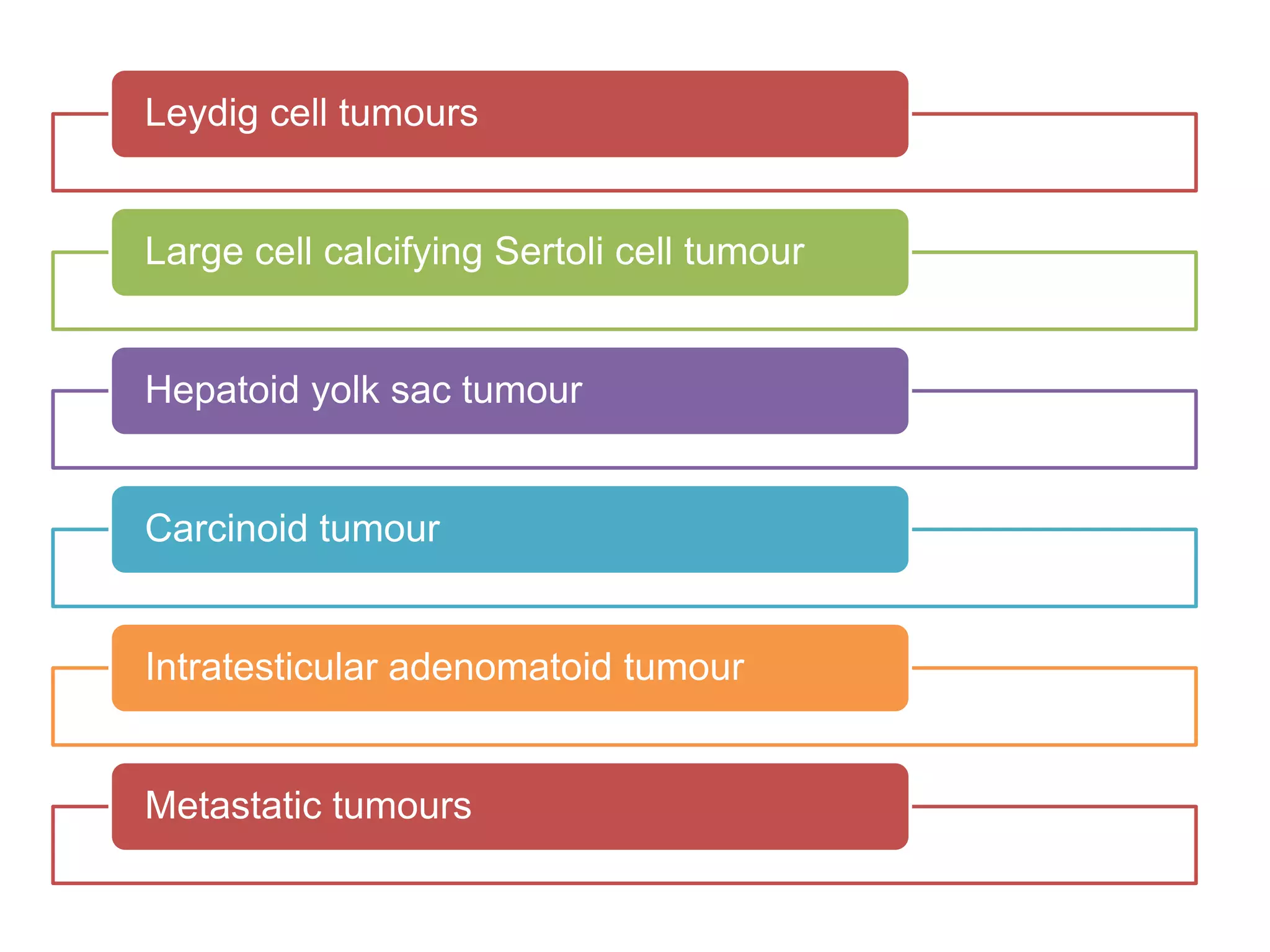
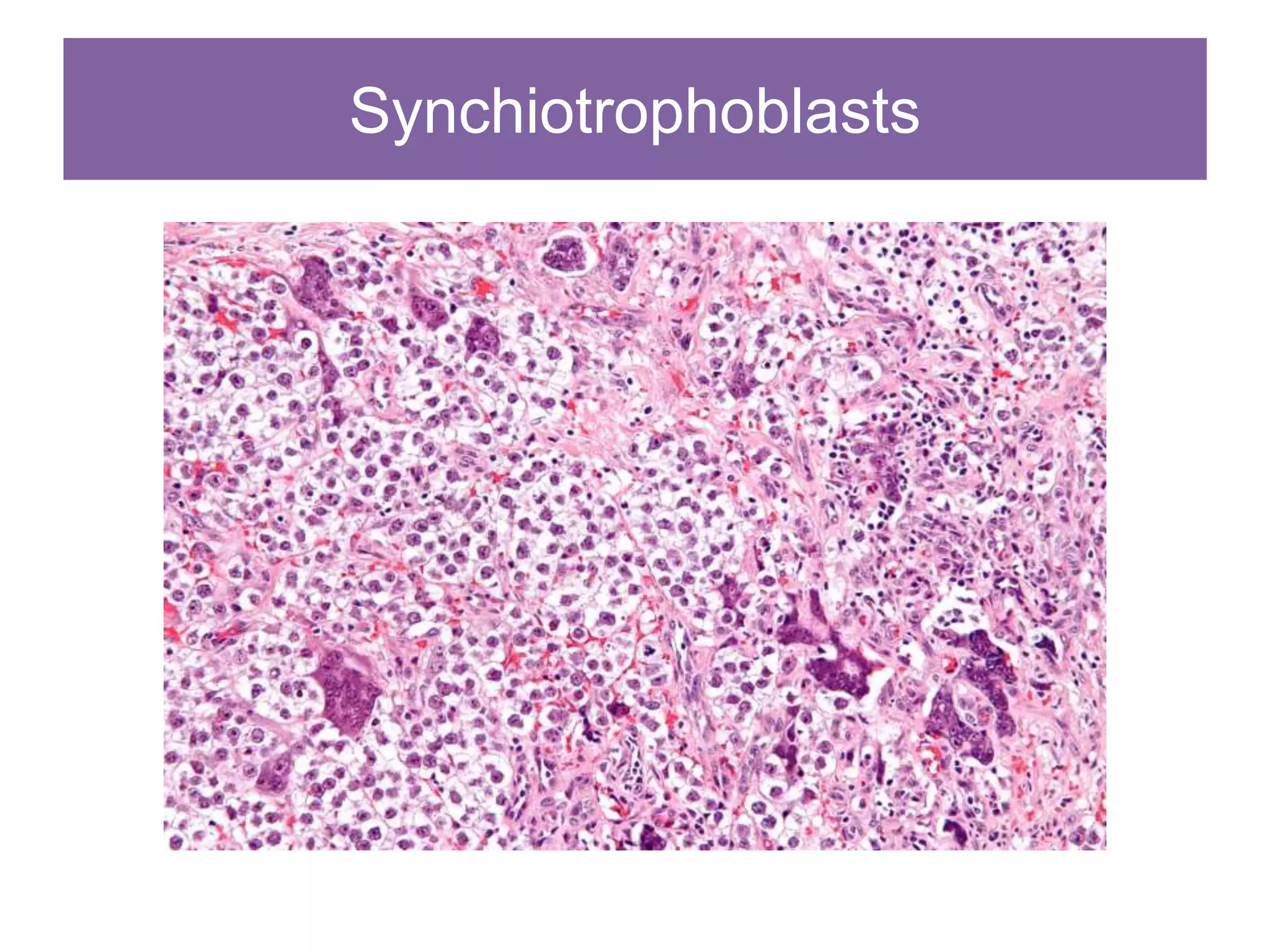
This document provides an overview of approaches to testicular tumors. It discusses updates to classifications including changing ITGCN to GCNIS. A new classification system is presented that divides tumors into GCT derived from GCNIS, GCT unrelated to GCNIS, sex cord stromal tumors, and other rare tumors. Factors like age, medical history, tumor site, and gross appearance can provide clues before histological examination. Histological patterns including cells with pale cytoplasm, glandular/tubular patterns, microcystic patterns, and oxyphilic cells can indicate tumor types.