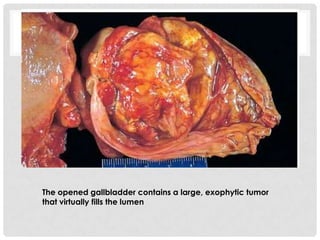
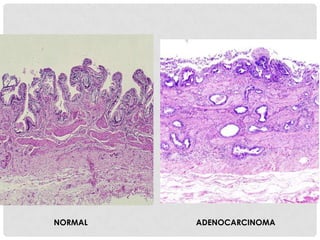
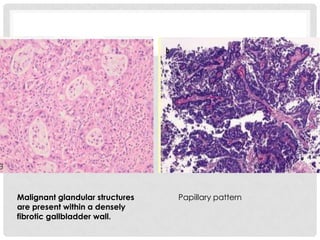
Carcinoma of the gallbladder is the most common malignancy of the extrahepatic biliary tract. It occurs most frequently in the seventh decade of life and has a poor 5-year survival rate of around 5-12% despite surgical intervention. The most important risk factor is gallstones, present in 95% of cases. Carcinomas of the gallbladder show infiltrating or exophytic patterns of growth and are usually adenocarcinomas, though some are squamous cell carcinomas. They typically invade the liver and involve lymph nodes by the time of discovery.