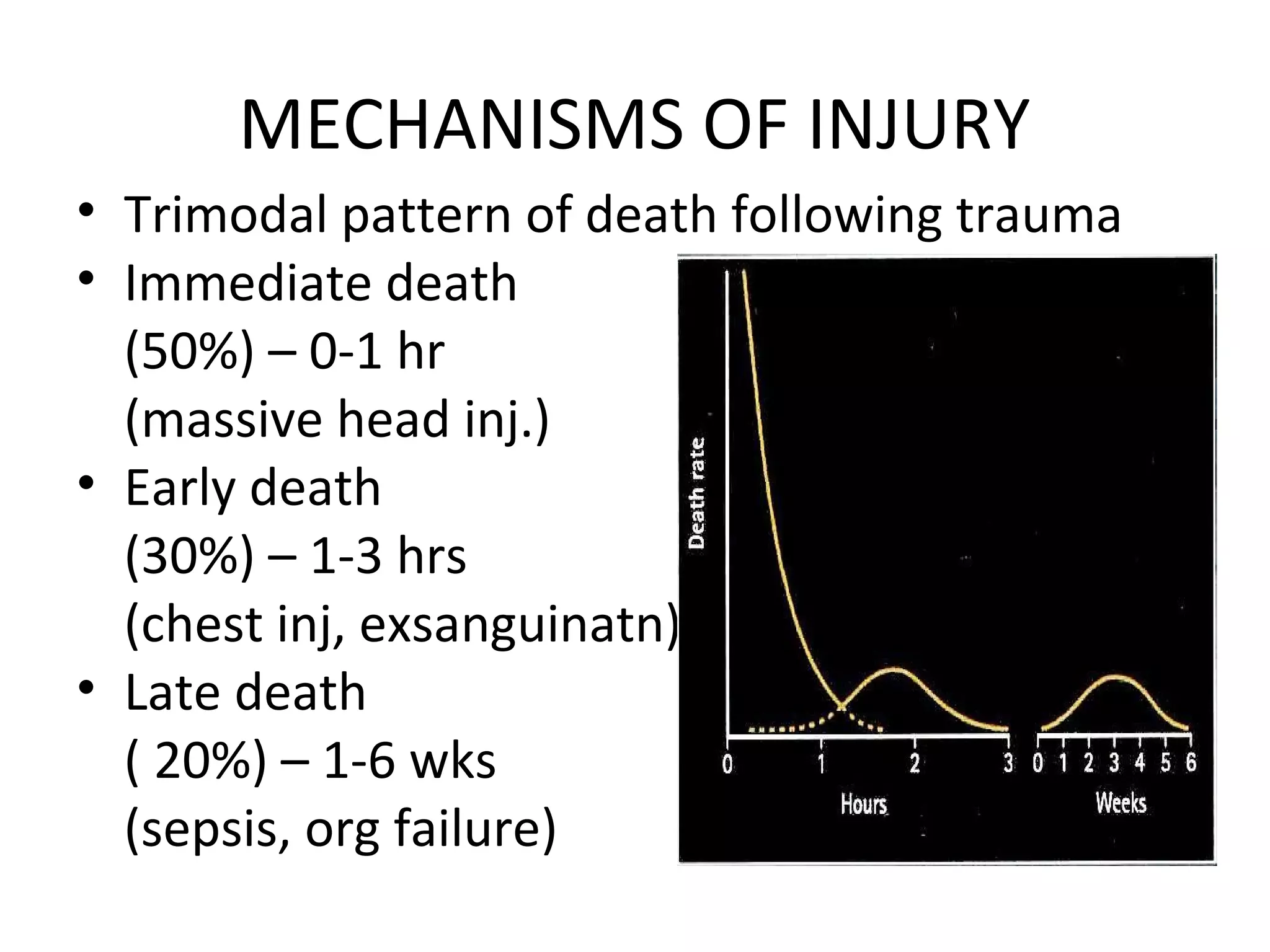
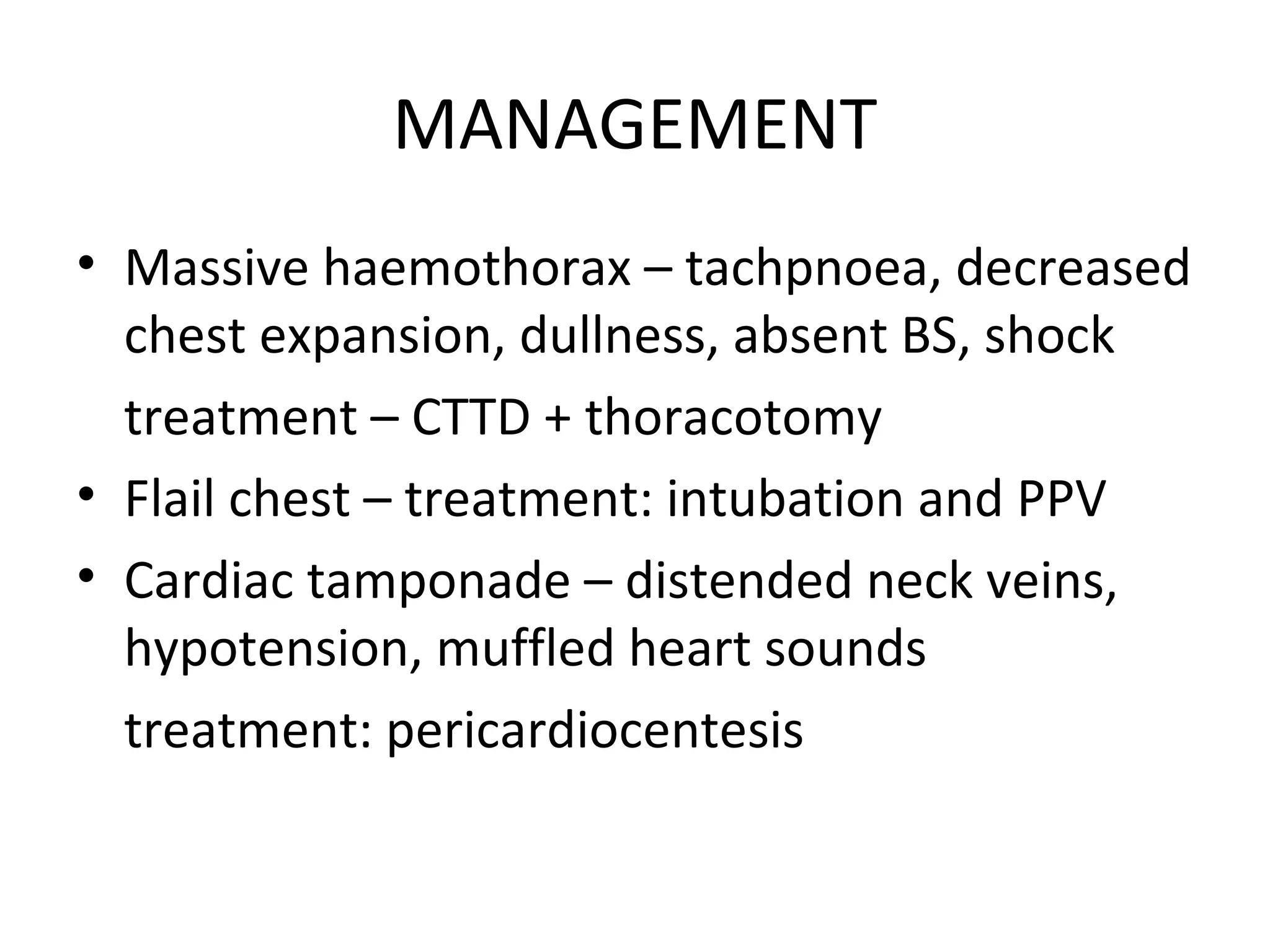
This document discusses the management of polytraumatized patients presenting to the emergency department. It defines polytrauma as two or more significant injuries to two or more organ systems. The management involves a multidisciplinary team performing a primary survey to address life threats, secondary survey to identify all injuries, and definitive treatment tailored to the patient's condition. Complications can include shock, sepsis, multiple organ dysfunction syndrome, and death if not properly managed. Special considerations are given to polytrauma in children, elderly, and pregnant patients.