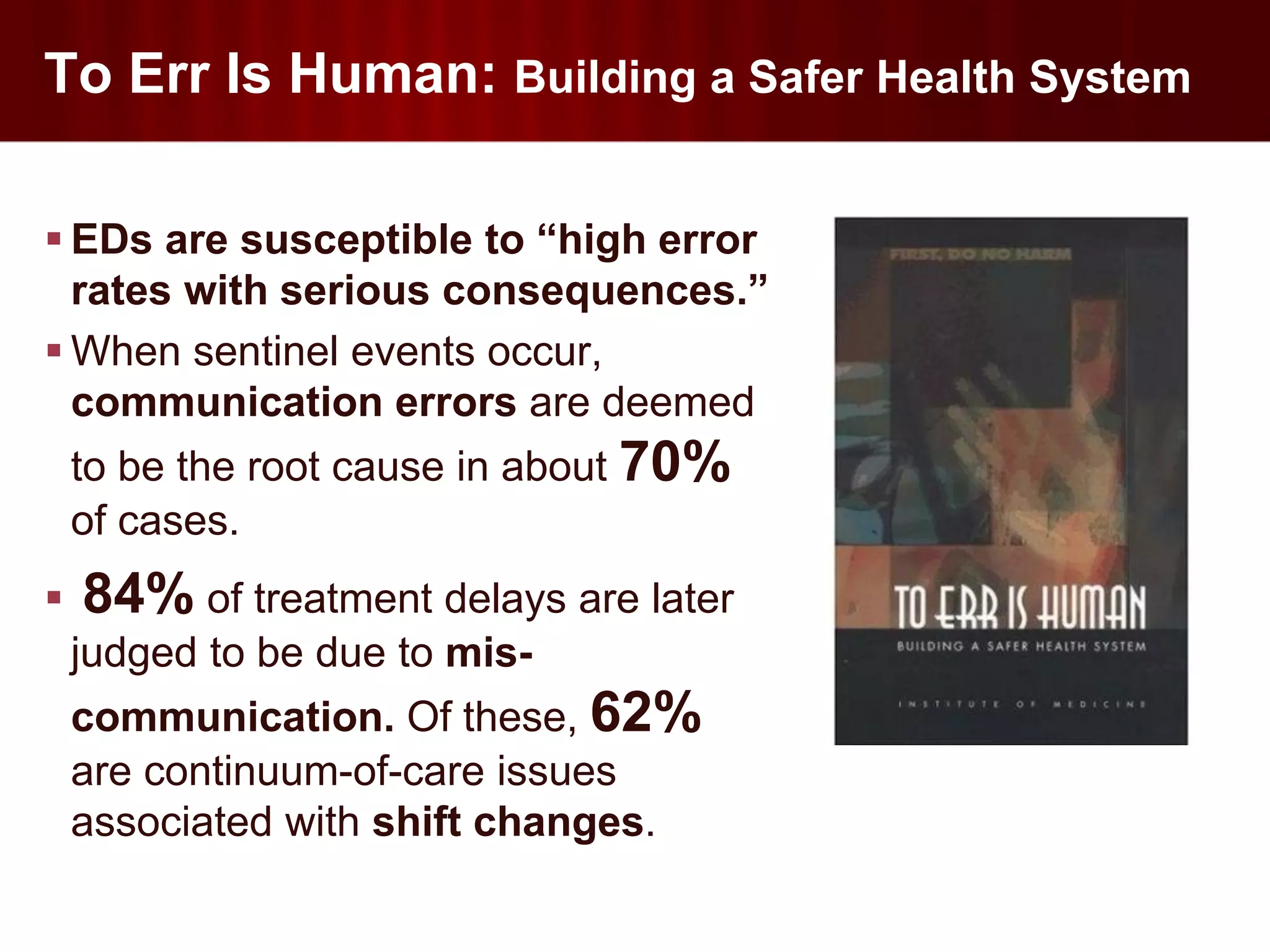
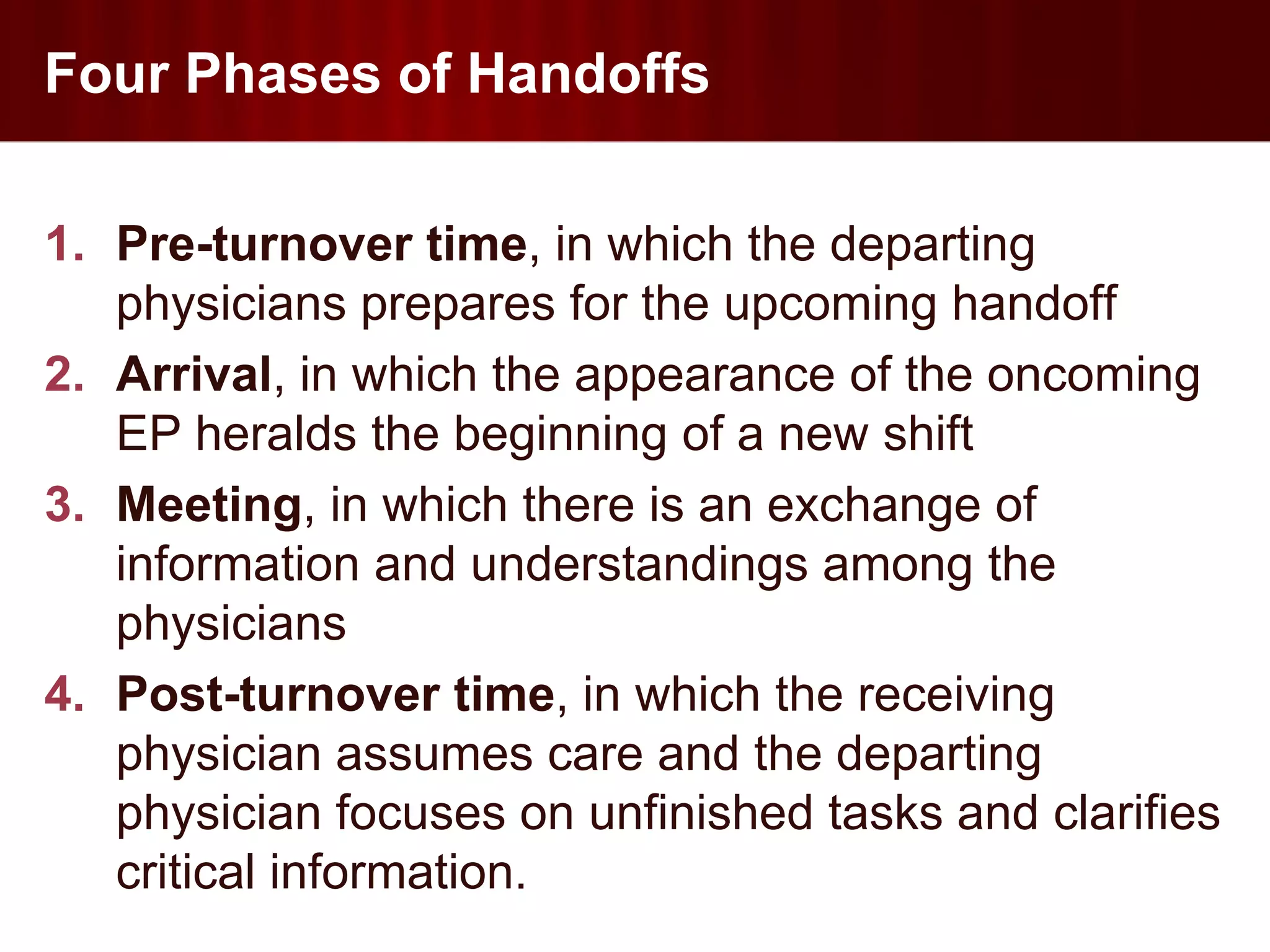
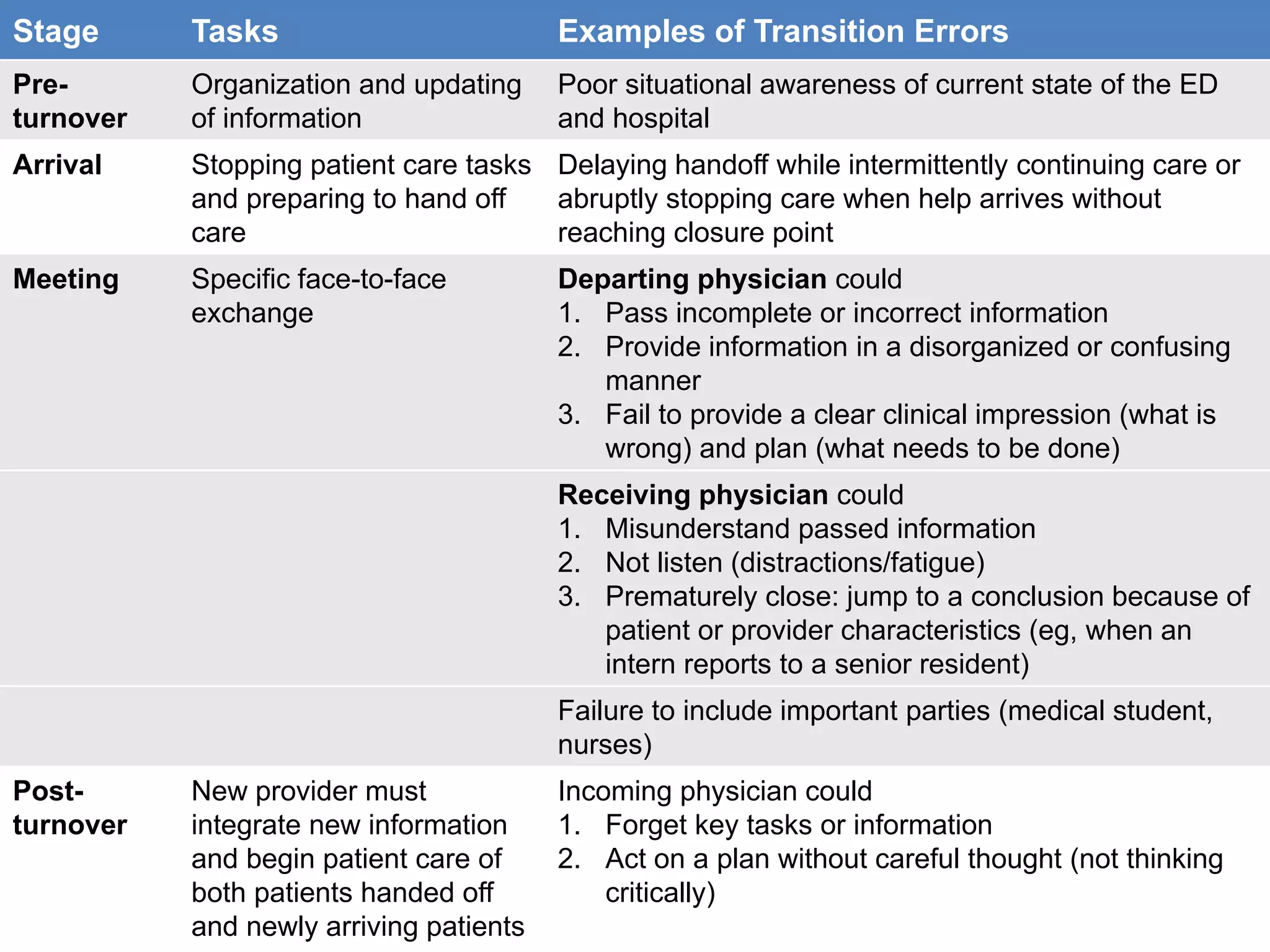
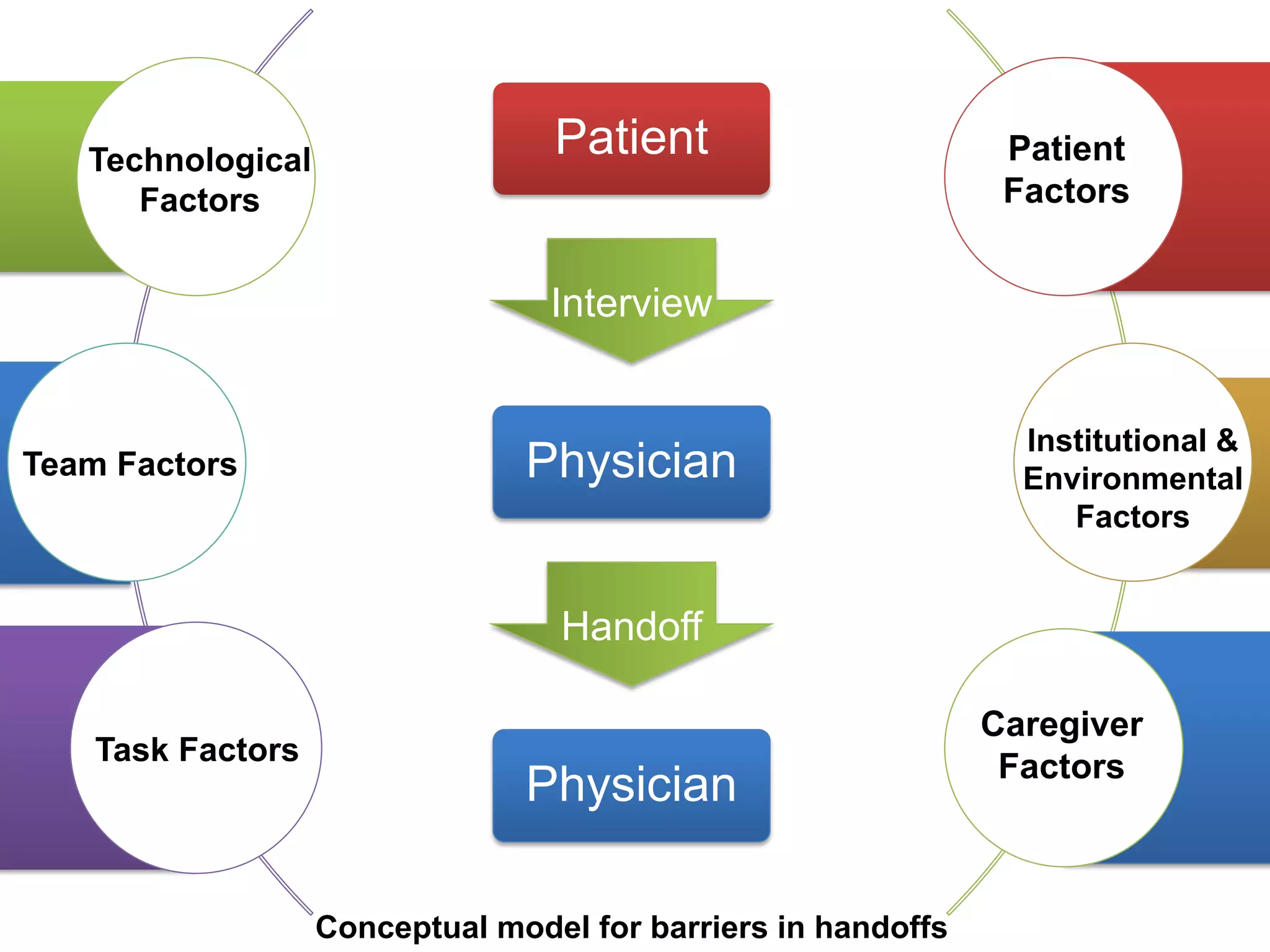
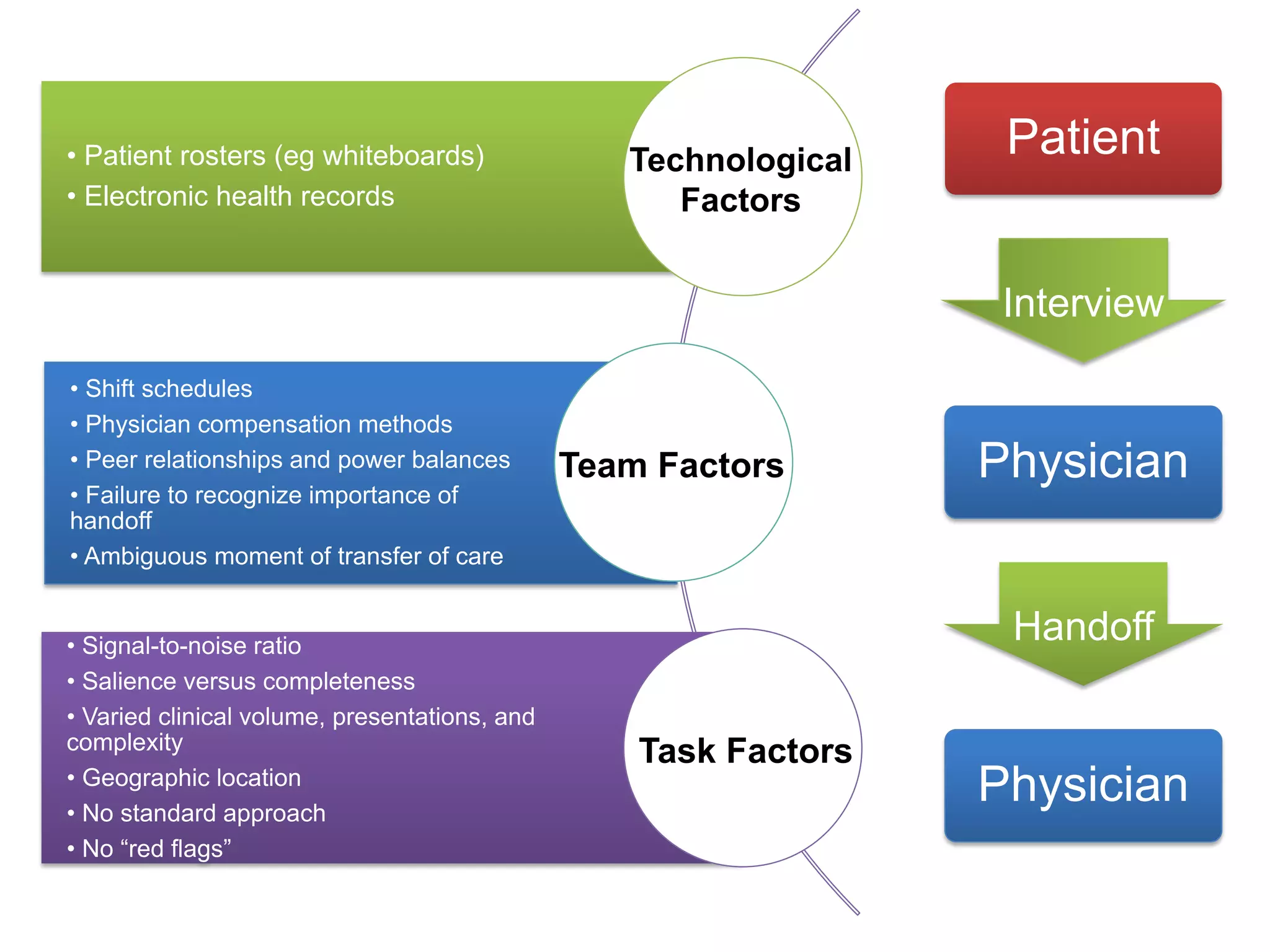
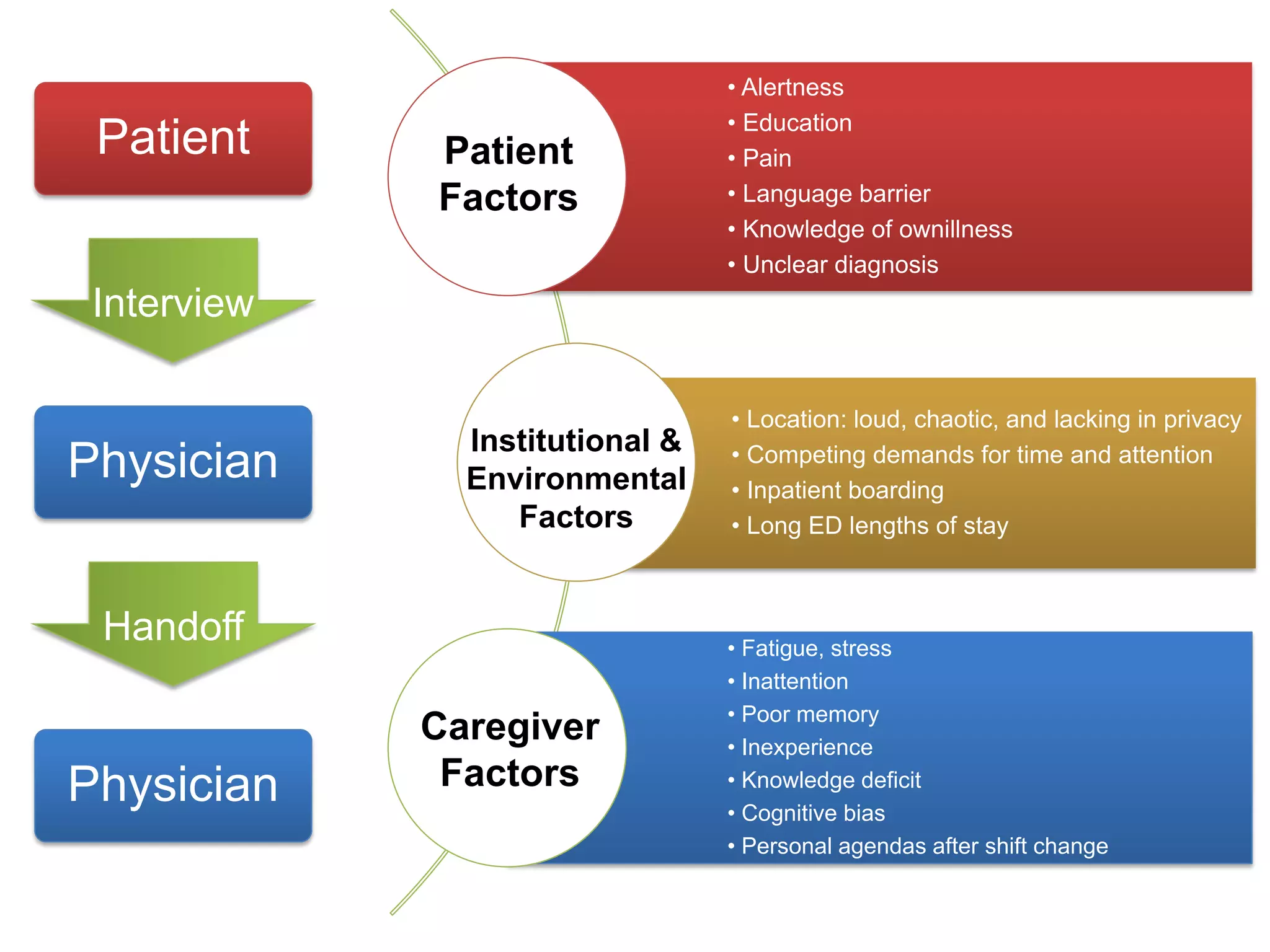
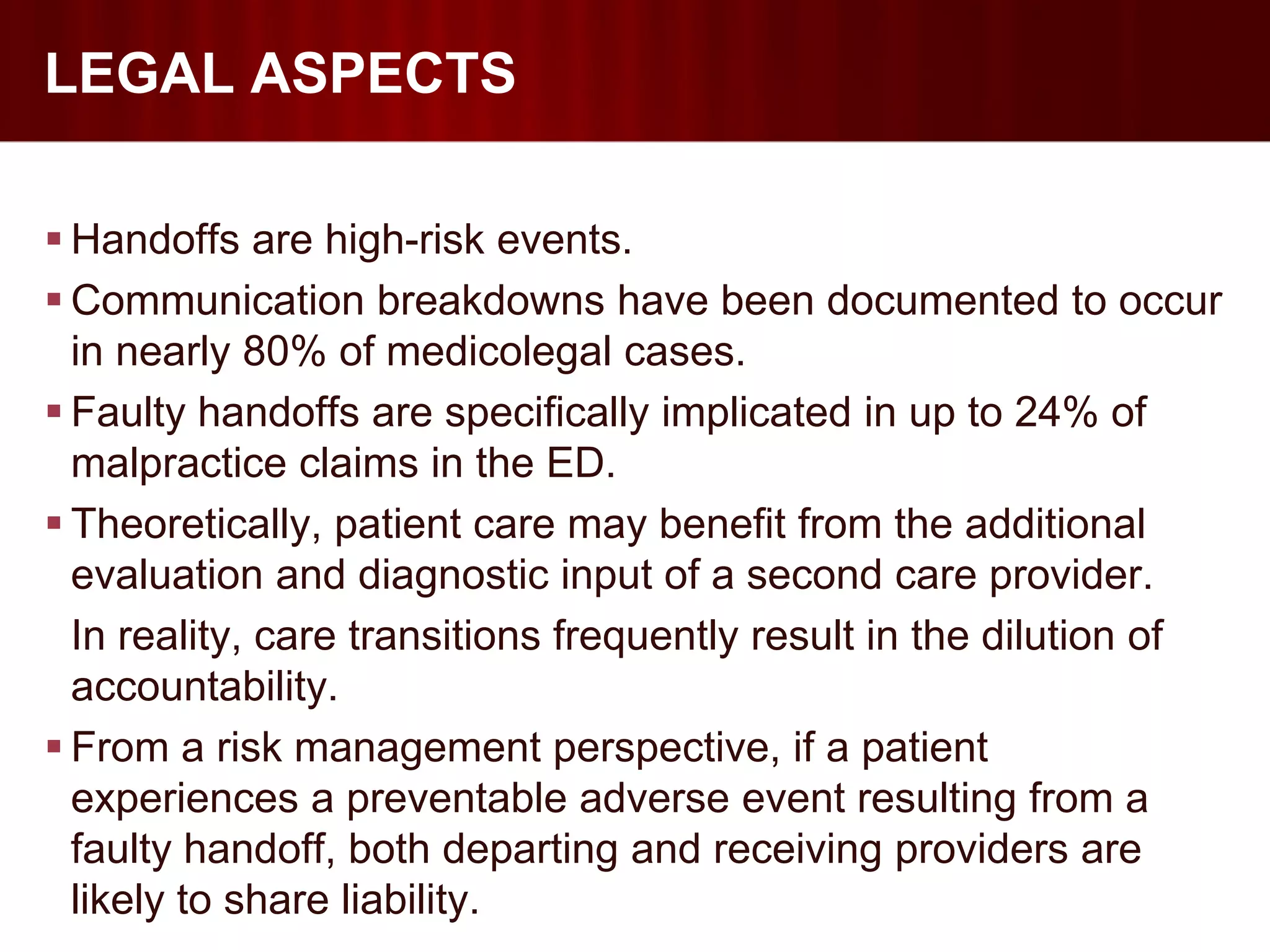
This document discusses improving handoffs between physicians in the emergency department. It notes that communication errors during shift changes are a common cause of treatment delays and adverse events. The document then reviews factors that can lead to errors during handoffs, including distractions, lack of standard processes, fatigue and inexperience. It proposes using multidisciplinary handoffs, clear guidelines and identifying high-risk patients to help improve safety during physician shift changes in the emergency department.