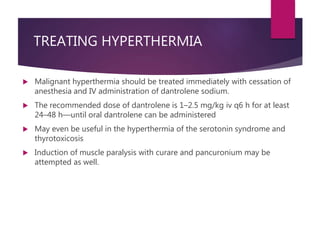
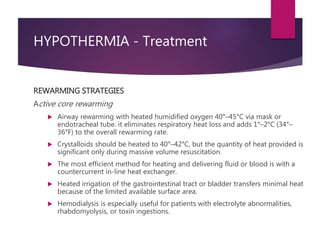
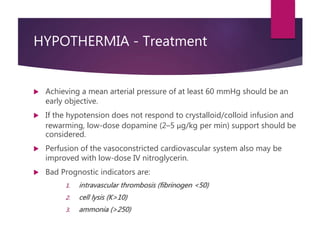
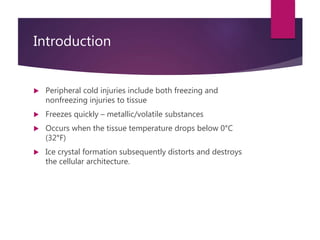
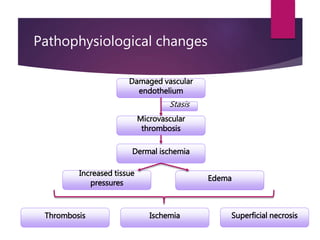
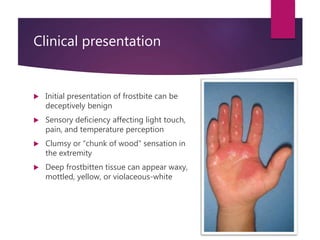
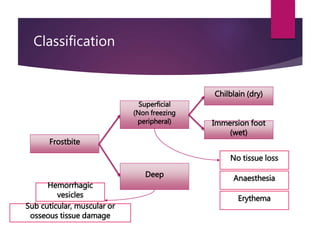
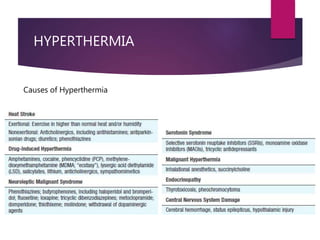
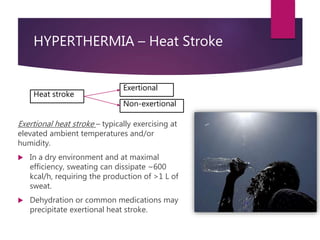
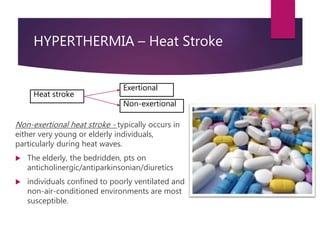
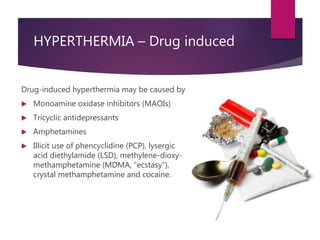
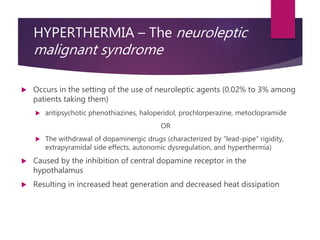
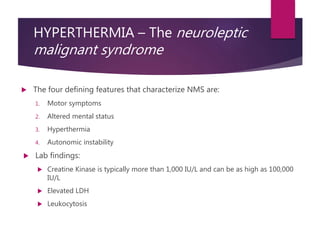
The document discusses temperature regulation disorders, including fever, hyperthermia, and hypothermia. It explains the physiological mechanisms behind these conditions, their causes, clinical presentations, and treatment strategies. Additionally, it covers complications like drug-induced hyperthermia and frostbite, highlighting preventive measures and approaches for managing severe cases.

![TREATING HYPERTHERMIA
In NMS - Supportive medical care, specific pharmacotherapy and electroconvulsive
therapy
Intensive monitoring and supportive treatment need admission to the intensive care unit
Discontinue neuroleptic agent or precipitating drug
Maintain cardiorespiratory stability.
Mechanical ventilation, antiarrhythmic agents
Maintain euvolemic state using intravenous (IV) fluids
If CK is very elevated, high volume IV fluids and urine alkalinization with IV sodium
bicarbonate [Na(HCO3)] may help to prevent renal failure from rhabdomyolysis.
Lower the temperature using cooling blankets, ice cold water, gastric lavage and ice
packets in axilla and cold sponging.
Lower BP, if markedly elevated (Clonidine)
LMWH for DVT prevention
Use benzodiazepines (clonazepam or lorazepam) to control agitation if necessary](https://image.slidesharecdn.com/temperatureregulationdisorders-160507100055/85/Temperature-regulation-disorders-20-320.jpg)