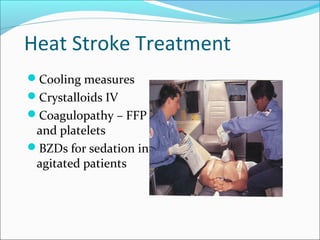
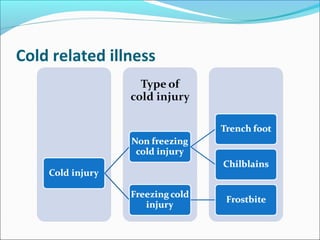
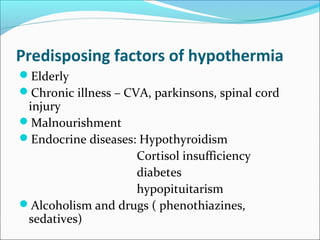
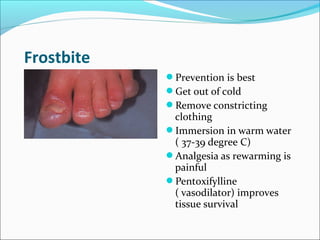
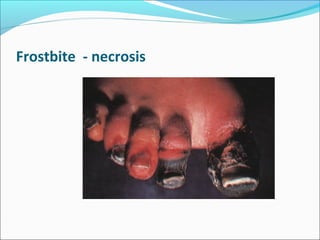
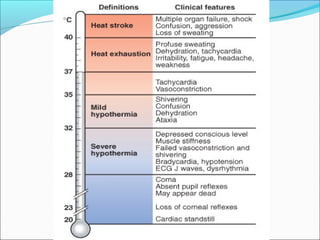
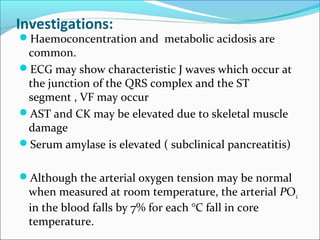
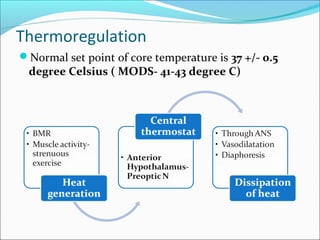
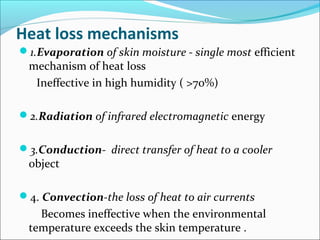
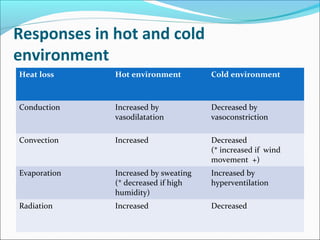
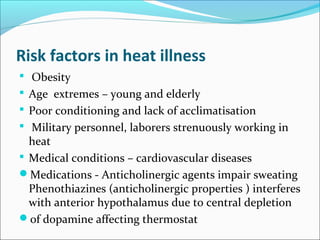
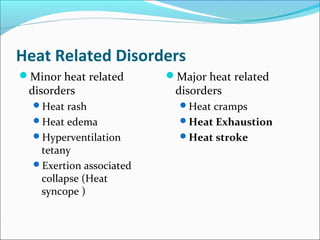
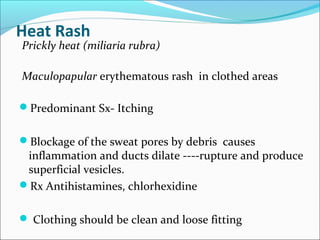
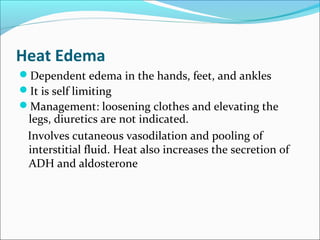
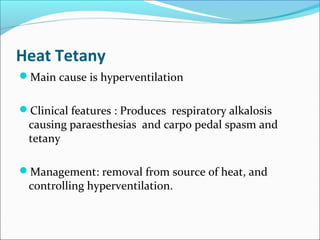
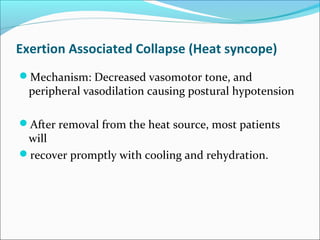
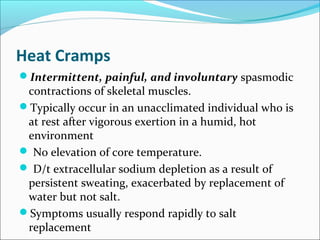
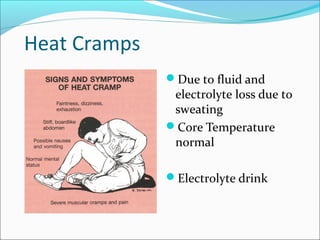
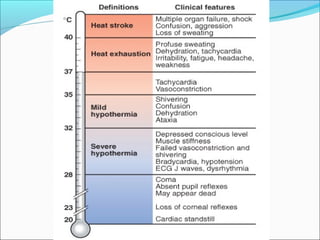
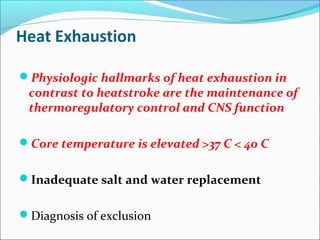
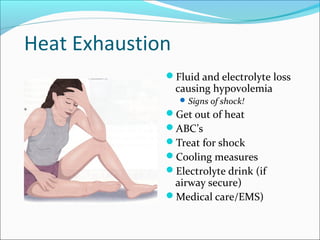
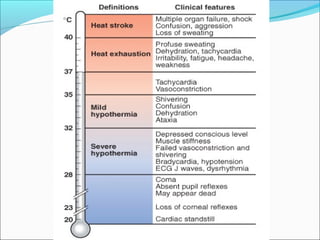
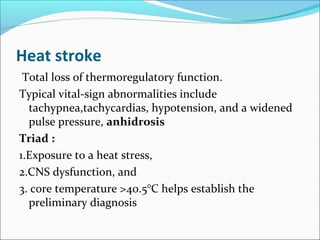
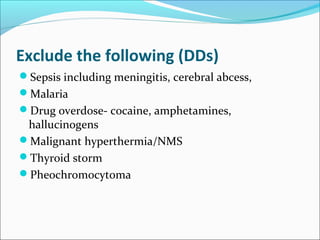
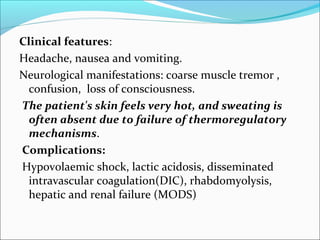
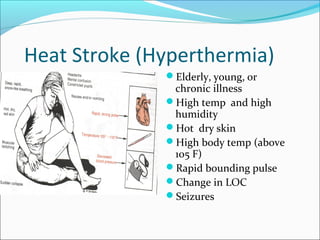
The document provides information on thermoregulation and illnesses related to heat and cold exposure. It discusses the normal mechanisms of heat loss and gain and how they are affected by hot and cold environments. Various minor and major heat-related illnesses like heat rash, heat exhaustion and heat stroke are described. The risks, signs, symptoms and management of these conditions are outlined. Cold-related injuries like frostbite and hypothermia are also summarized, including treatments like gradual rewarming. Investigations for hypothermia and approaches for mild versus severe hypothermia are highlighted.
![Cooling tecniques
Spraying Cool water (15°C [60° F]) on exposed skin
Fans direct continuous airflow over the moistened
skin.
Cold packs applied to the axillae and groin
Safety of Immersion cooling (only for young,
previously healthy patients )](https://image.slidesharecdn.com/heatandcoldinjuries-170820051800/85/Heat-and-cold-injuries-24-320.jpg)