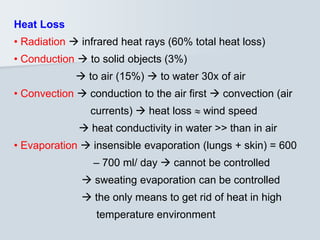
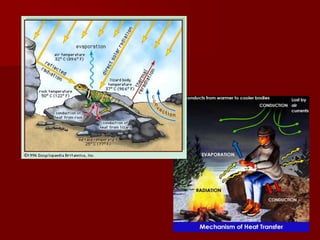
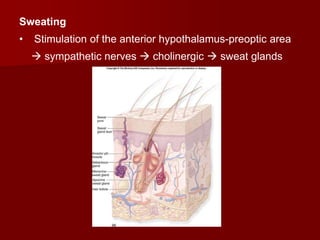
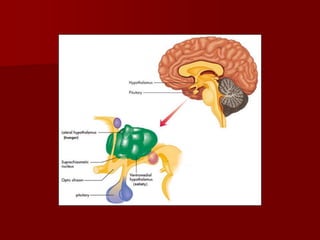
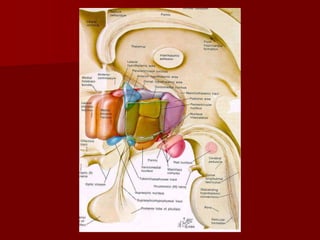
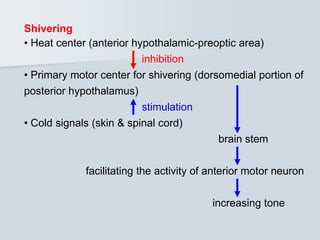
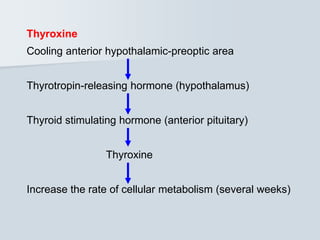
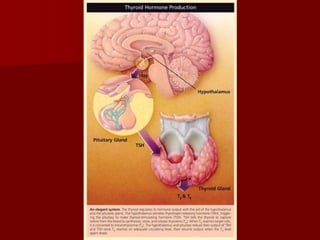
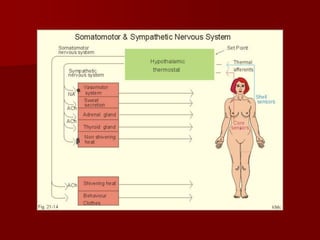
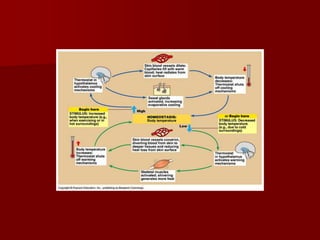
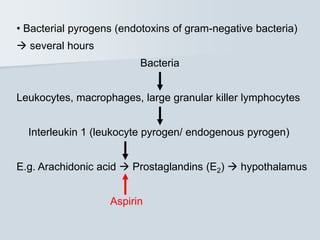
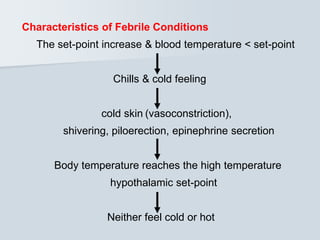
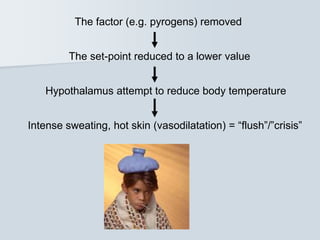
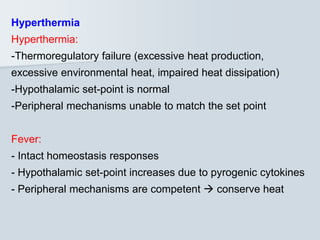
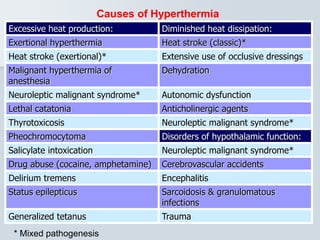
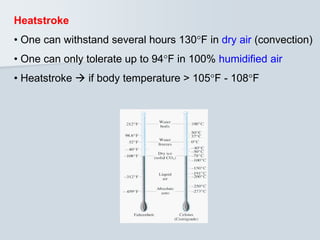
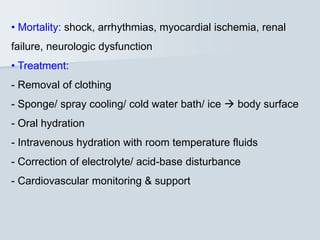
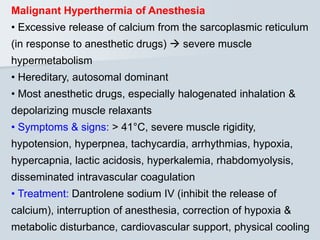
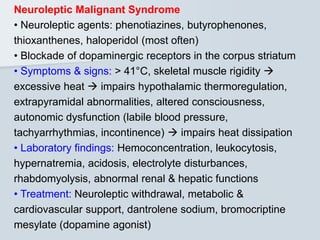
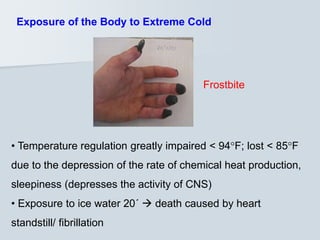
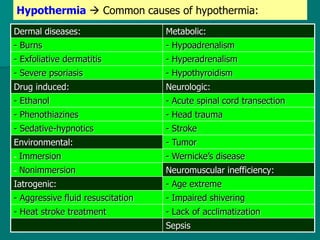
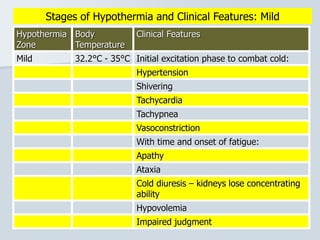
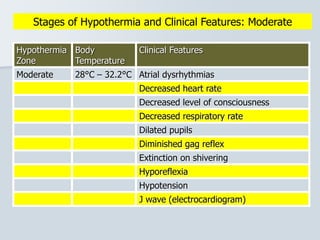
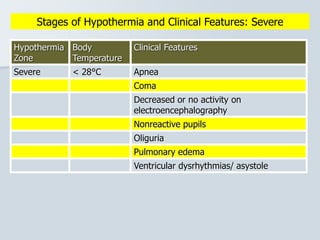
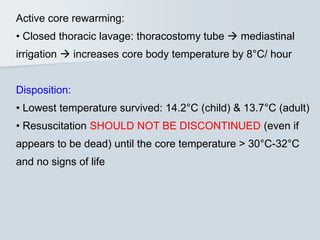
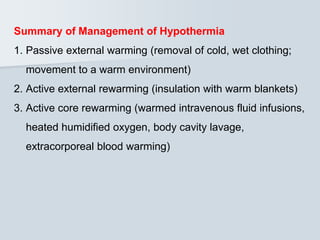
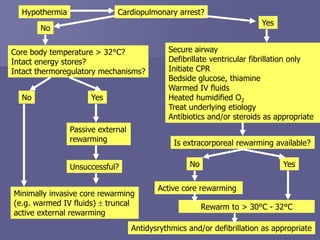
The document discusses thermoregulation and body temperature control, highlighting the balance between heat production and heat loss mechanisms. It explains physiological processes involved in temperature regulation, including the roles of the hypothalamus, skin receptors, and various responses to cold and heat stimuli. Additionally, it covers the implications of temperature abnormalities such as hyperthermia and hypothermia, their causes, clinical features, and management strategies.