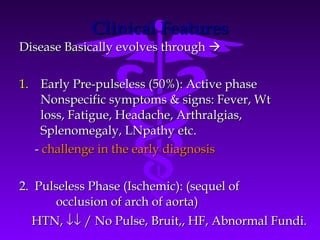
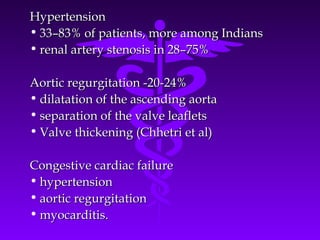
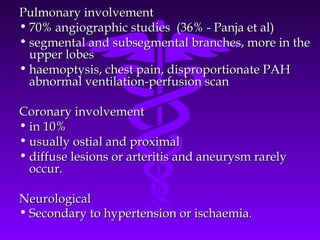
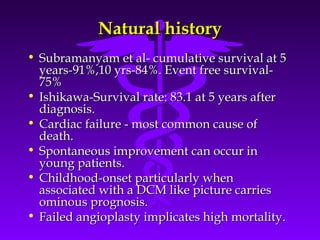
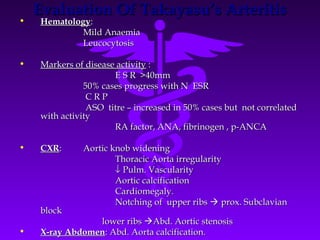
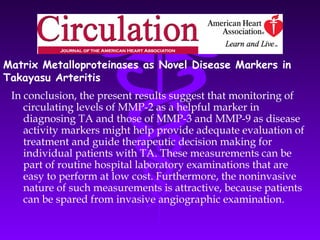
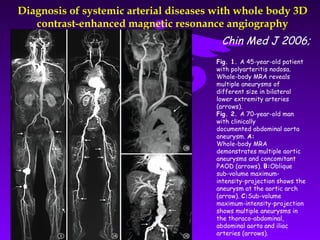
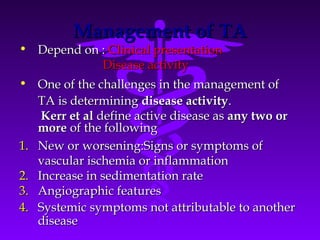
Takayasu arteritis is an idiopathic inflammatory disease that primarily affects large elastic arteries, especially the aorta and its branches. It most commonly occurs in young females. The disease involves occlusive or ectatic changes in the arteries and can present with nonspecific early symptoms or later with signs of ischemia due to arterial occlusion. Diagnosis is based on criteria that consider clinical features, imaging findings, and laboratory tests showing inflammation. Treatment involves management of symptoms and immunosuppression.





![OCULAR :
• Amaurosis fugax
• Hypertensive retinopathy [keith-wagner]
arteriolar narrowing, av crossing changes
silver wiring, exudates, papilloedema.
• Ischemic retinopathy [ Uyama and Asayama]
Stage 1 : dilatation of small vessels
stage 2 : micro aneurism formation
stage 3 : wreath like AV anastamosis
formation surrounding optic
papillae
stage 4 : cataract ,secondary glacoma
,rubeosis,
neo vascularisation, proliferative
retinopathy, vitreous hemorrhage.](https://image.slidesharecdn.com/takayasuarteritis-final-130120231806-phpapp02/85/Takayasu-arteritis-fin-al-31-320.jpg)




![Activity of disease
[clinical symptoms, ESR, angiography,biopsy]
Active disease Inactive disease
- Prednisolone 1 mg/kg ( 3 mon)
Remission Resistent
cyclo phosphamide 2mg/kg
Taper steroids methotrexate 20mg /wk
azathioprim 200mg/day
Persistent Relapse
remission](https://image.slidesharecdn.com/takayasuarteritis-final-130120231806-phpapp02/85/Takayasu-arteritis-fin-al-53-320.jpg)


![Infliximab is Effective for Takayasu
Arteritis Refractory to
Glucocorticoid and Methotrexate
The pathogenesis of TA includes vessel injury due to products from activated T
cells, natural killer cells, γ/δ T cells and macrophages. One of the important
humoral factors is TNF-α, the molecular target for human autoimmune diseases
Glucocorticoid therapy is usually introduced for TA, but glucocorticoid alone is
sometimes not efficient; Kerr et al reported that about half of active TA patients
did not respond well to glucocorticoid alone (6). In addition to glucocorticoid, an
immunosuppressive regime such as cyclophosphomide, methotrexate and
azathioprine has been used to treat TA (6-8); however, some patients are
refractory to both glucocorticoid and immunosuppressants. Hoffman et al have
recently reported the efficacy of TNF blockers toward TA refractory to
conventional glucocorticoid therapy and immunosuppressants Patient selection
criteria described by Hoffman et al include:1] required toxic doses of
glucocorticoids to maintain remission, and 2] either experienced multiple
relapses while receiving conventional and experimental therapy or refused re-
treatment with glucocorticoids following relapses](https://image.slidesharecdn.com/takayasuarteritis-final-130120231806-phpapp02/85/Takayasu-arteritis-fin-al-57-320.jpg)