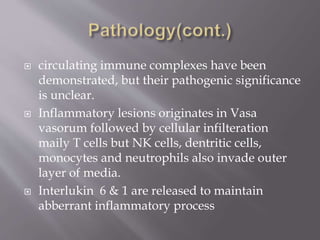
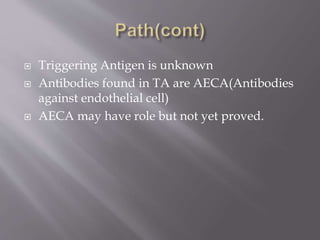
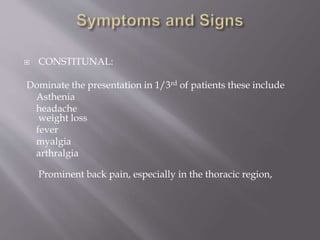
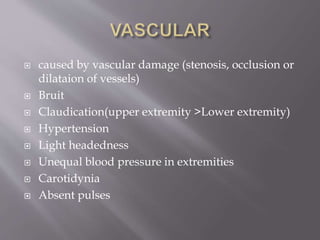
Takayasu arteritis is a chronic inflammatory disease that causes stenosis, occlusion, dilation or aneurysm of the aorta and its branches. It most commonly affects adolescent girls and young women. Symptoms include limb claudication, decreased brachial pulse, hypertension, bruits, and vascular ischemia. Diagnosis is based on meeting criteria such as age of onset under 40, decreased pulse, blood pressure difference between arms, and angiographic evidence of vascular involvement. Treatment involves glucocorticoids which can control inflammation and symptoms, though relapses may occur. Additional immunosuppressants may be needed, and management of hypertension is important, especially during pregnancy which carries higher risks but fertility is not affected.