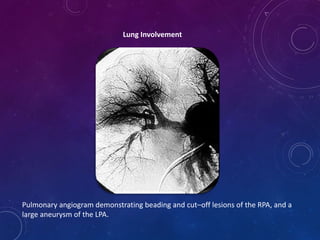
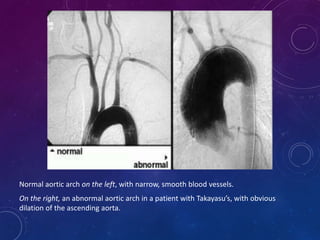
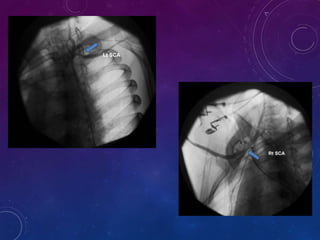
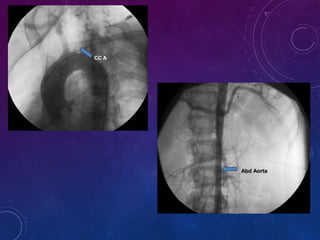
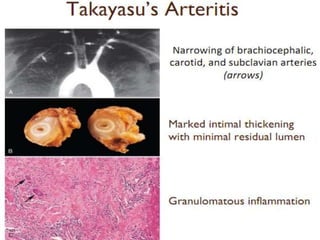
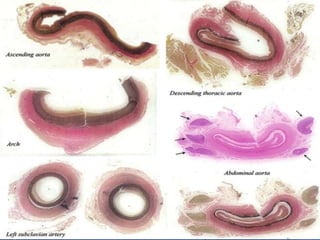
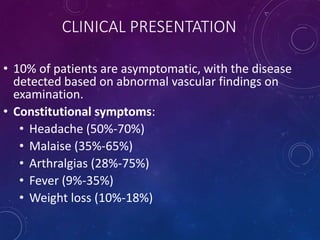
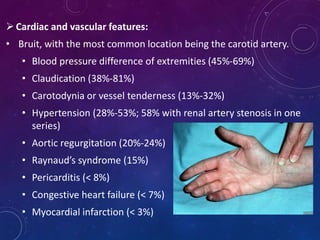
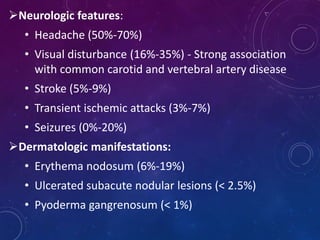
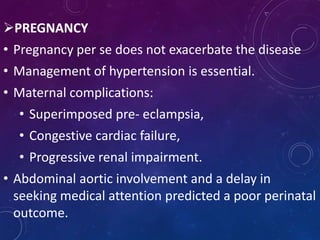
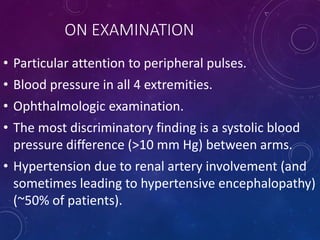
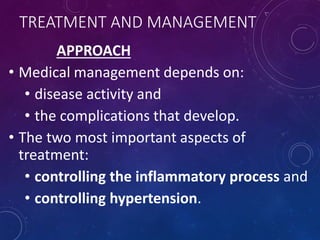
Takayasu's arteritis is a rare inflammatory disease that affects large blood vessels. It most commonly involves the aorta and its major branches. It predominantly affects young women of Asian descent. Symptoms can include headaches, fatigue, joint pains, and abnormalities in blood pressure between limbs. Diagnosis involves imaging tests like angiograms to detect vessel narrowing, blockages, or aneurysms. Treatment focuses on controlling inflammation with corticosteroids and immunosuppressants, and managing hypertension through cardiovascular procedures or surgery if needed. Strict control of risk factors is also important to prevent complications like heart disease.
![Anti-tumor necrosis factor agents
• Used in relapsing disease.
• Initial dose of etanercept was 25 mg twice weekly (7
patients);
infliximab (11 patients [3 were switched from
etanercept to infliximab]) was given at 3 mg/kg initially
and at 2 weeks, 6 weeks, and then every 8 weeks
thereafter.
In 9 of the 14 responders, an increase in the anti-TNF
dosage was required to sustain remission.](https://image.slidesharecdn.com/takayasusarteritis-171226162041/85/Takayasusarteritis-28-320.jpg)