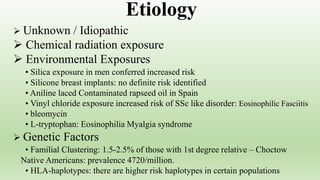
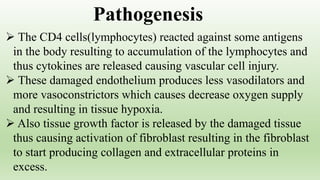
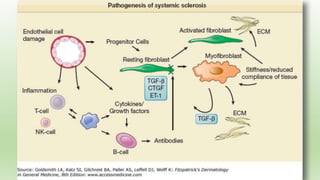
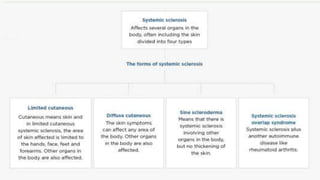
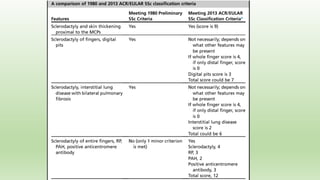
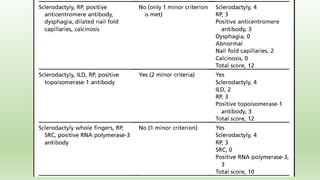
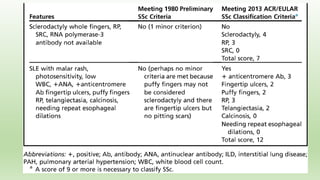
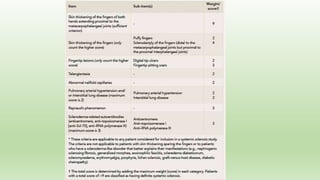
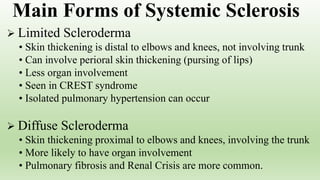
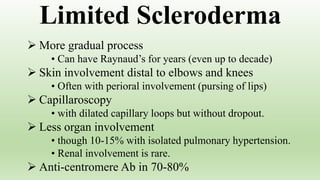
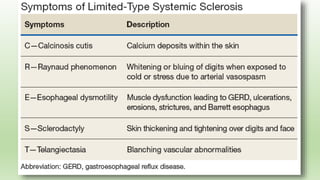
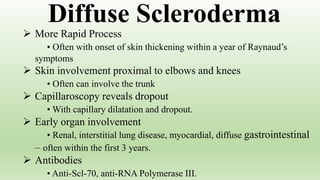
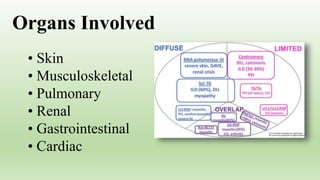
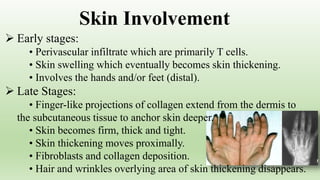
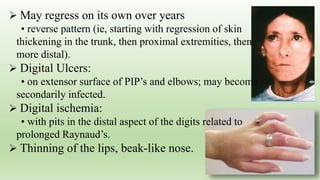
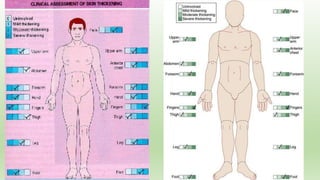
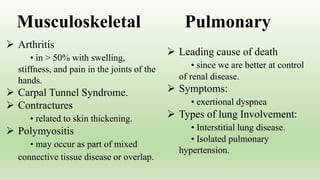
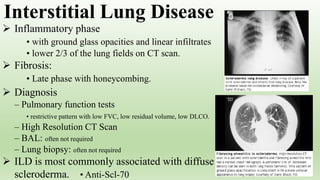
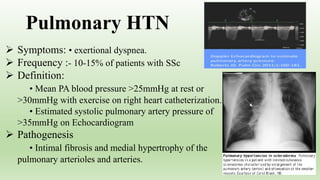
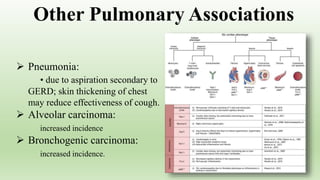
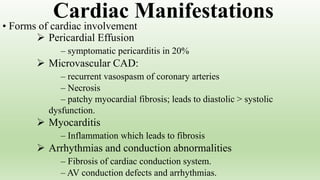
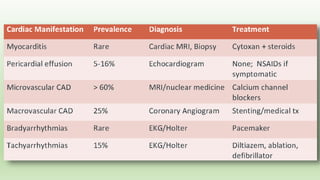
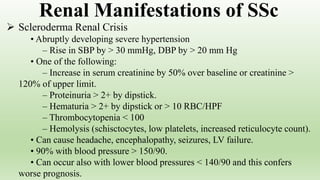
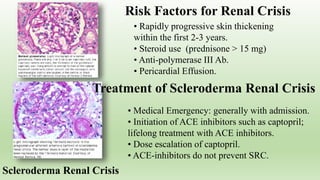
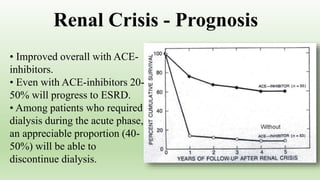
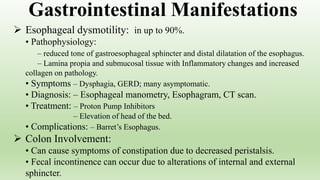
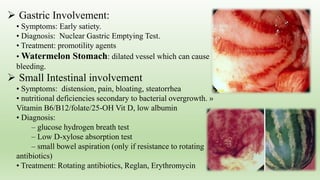
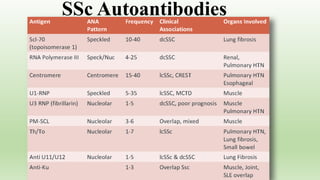
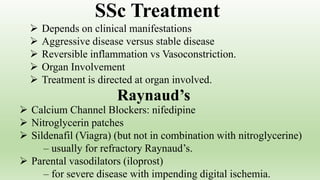
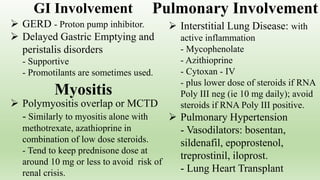
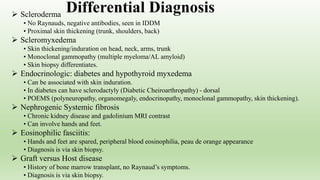
Systemic sclerosis (SSc) is a multisystem disorder characterized by skin thickening, with a peak incidence in women aged 35-64. The etiology remains largely unknown, involving both environmental and genetic factors, and presents as limited or diffuse forms with varied organ involvement. Treatment focuses on managing symptoms and complications across affected systems, including pulmonary, renal, and gastrointestinal manifestations.