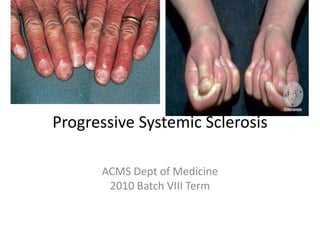
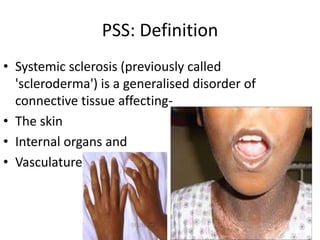
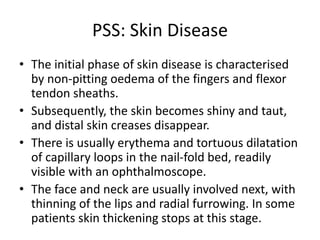
Progressive systemic sclerosis is a disorder affecting connective tissue in the skin, internal organs, and blood vessels. It is characterized by thickening and tightening of the skin, especially in the fingers and face. It can be classified as limited or diffuse cutaneous disease depending on the extent of skin involvement. Internal organ systems commonly impacted include the lungs, heart, kidneys, and gastrointestinal tract. Management involves treatments for symptoms such as Raynaud's phenomenon, digital ischemia, reflux, and pulmonary hypertension. Prognosis depends on factors like the extent of skin and organ involvement.