The document discusses the case of Nahid, a 29-year-old woman diagnosed with systemic lupus erythematosus (SLE) after presenting with symptoms like joint pain and swelling. It outlines her clinical history, laboratory findings, and treatment approach, including medications for SLE manifestations and management of related complications. It further elaborates on the nature of SLE as a chronic inflammatory disease, its prevalence, clinical manifestations, and the recommended evaluations and therapeutic strategies.











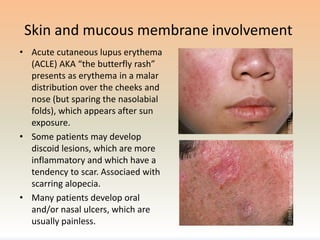


![Renal involvement
• Occur in ~50% of SLE patients, causes significant morbidity
& mortality.
• Periodic screening for lupus nephritis: [urinalyses,
quantitation of proteinuria, and eGFR] is an important
component of the ongoing management of SLE patients.
Several forms of glomerulonephritis can occur, and renal
biopsy is useful to define the type and extent of renal
involvement.
• Lupus nephritis can present as asymptomatic hematuria
and/or proteinuria to nephrotic syndrome and rapidly
progressive GN with loss of renal function. Some patients
with lupus nephritis also have hypertension.](https://image.slidesharecdn.com/approachtosle-181109093028/85/Approach-to-sle-15-320.jpg)





![Lab investigations:
• CBC w differential may reveal leukopenia, mild anemia, and/or thrombocytopenia
• Elevated serum creatinine may be suggestive of renal dysfunction
• Urinalysis with urine sediment may reveal hematuria, pyuria, proteinuria, and/or
cellular casts
In addition to the routine laboratories described above, we perform the following
laboratory tests which support the diagnosis of SLE if abnormal:
• ANA (+ve in virtually all SLE patients) If the ANA is positive, one should test for other
specific antibodies such as dsDNA, anti-Sm, Ro/SSA, La/SSB, and U1 ribonucleoprotein
(RNP).
• Antiphospholipid antibodies (lupus anticoagulant [LA], IgG and IgM anticardiolipin [aCL]
antibodies; and IgG and IgM anti-beta2-glycoprotein [GP] I)
• C3 and C4 or CH50 complement levels
• Erythrocyte sedimentation rate (ESR) and/or C-reactive protein (CRP) levels
• Urine protein-to-creatinine ratio](https://image.slidesharecdn.com/approachtosle-181109093028/85/Approach-to-sle-21-320.jpg)


















![NONIMMUNOSUPPRESSIVE THERAPY
• Aggressive antihypertensive and, in patients
with proteinuria, antiproteinuric therapy with
blockade of the renin-angiotensin system (eg,
angiotensin-converting enzyme [ACE] inhibitor
or angiotensin II receptor blocker [ARB]).
• Lipid lowering with statin therapy (CKD >
cardiovascular mobidity & mortality).](https://image.slidesharecdn.com/approachtosle-181109093028/85/Approach-to-sle-41-320.jpg)






