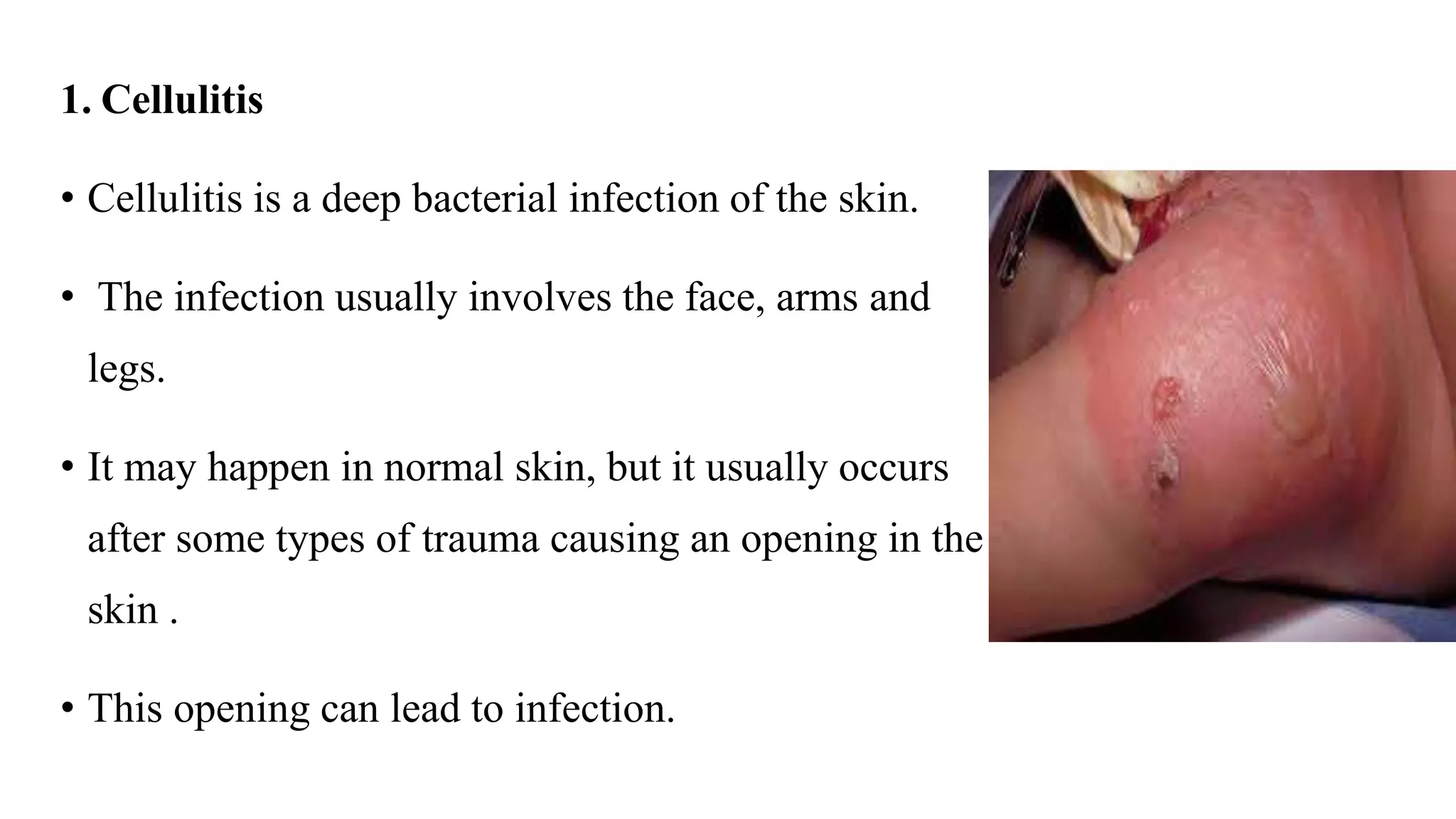
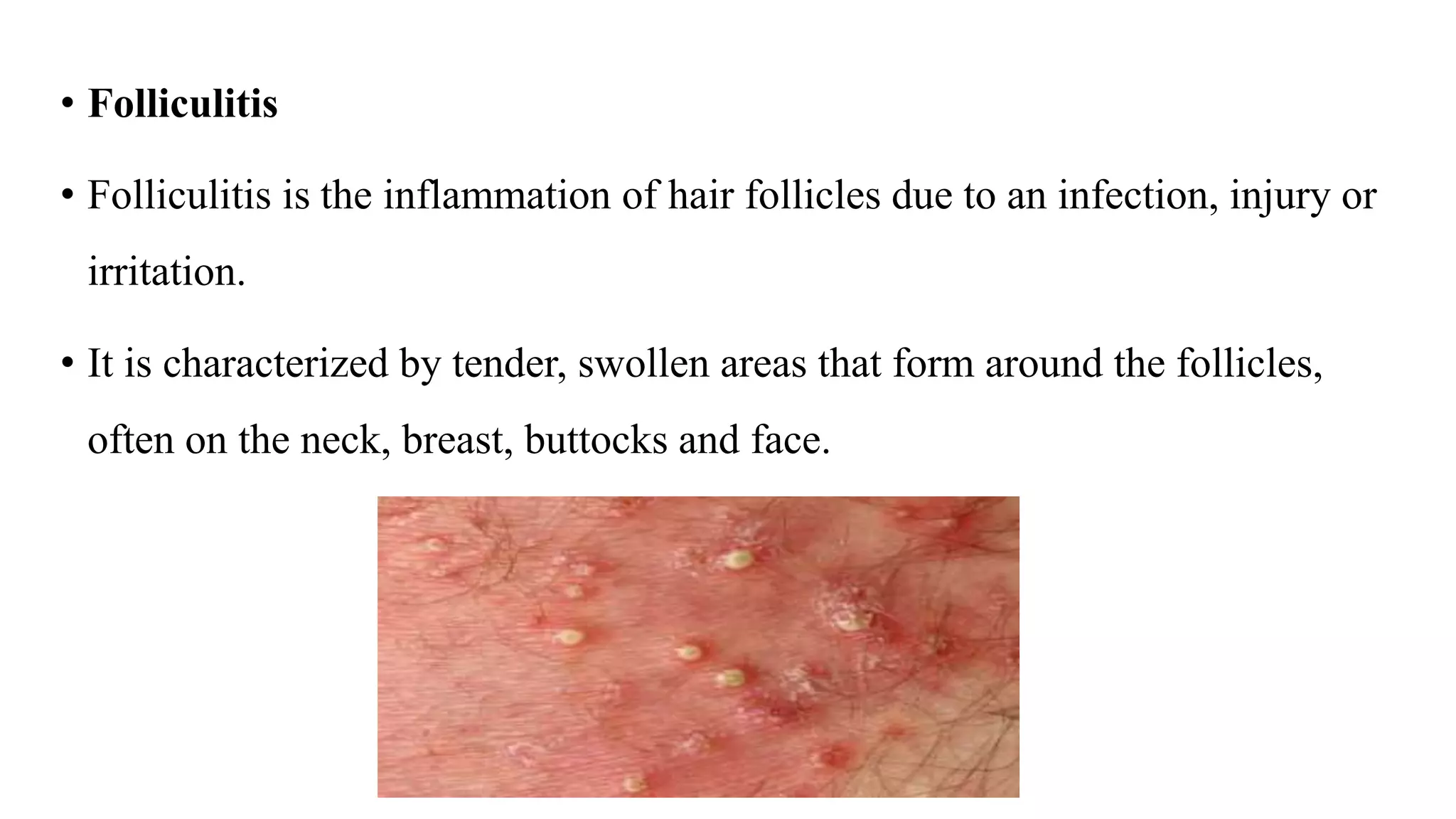
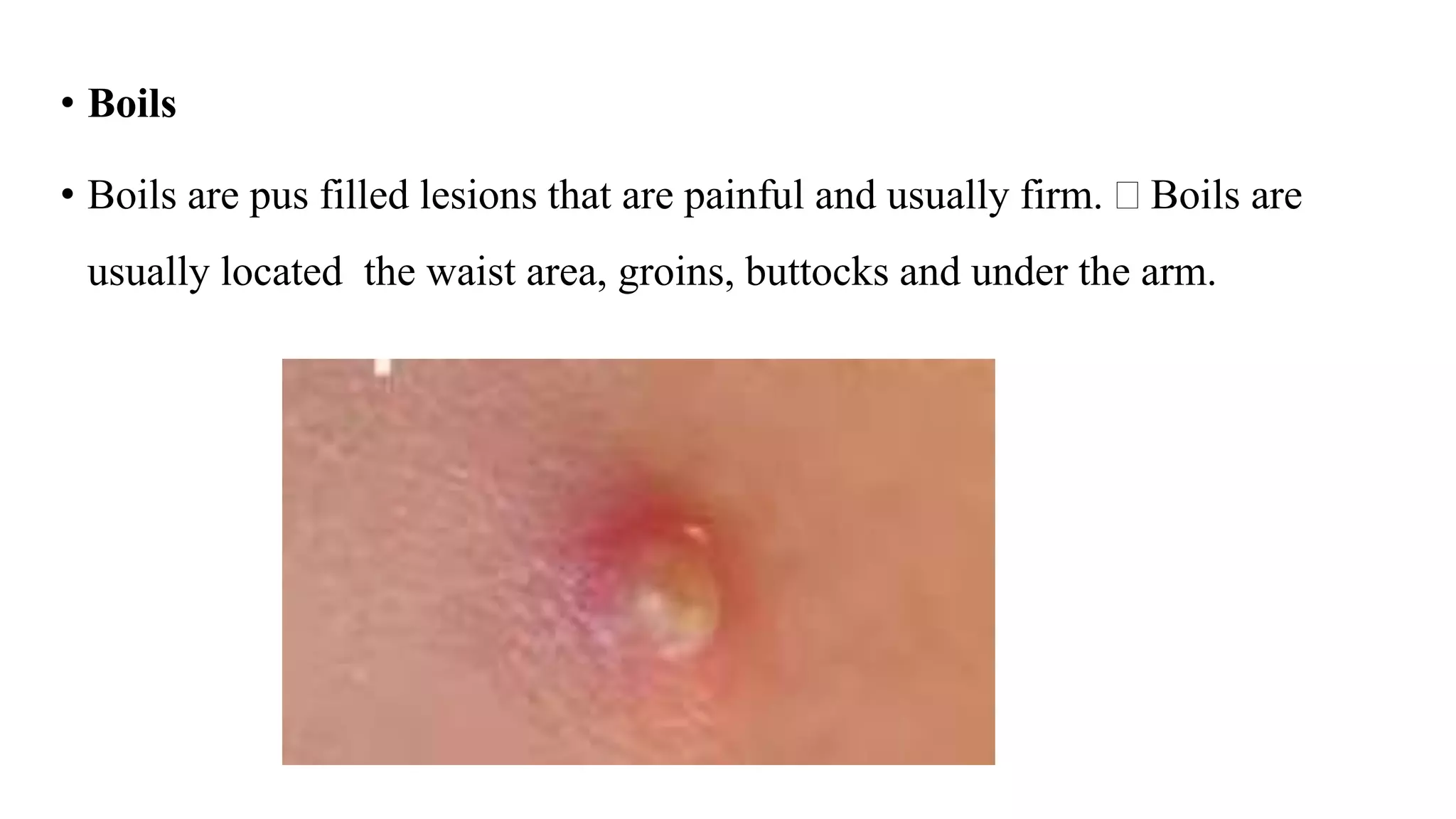
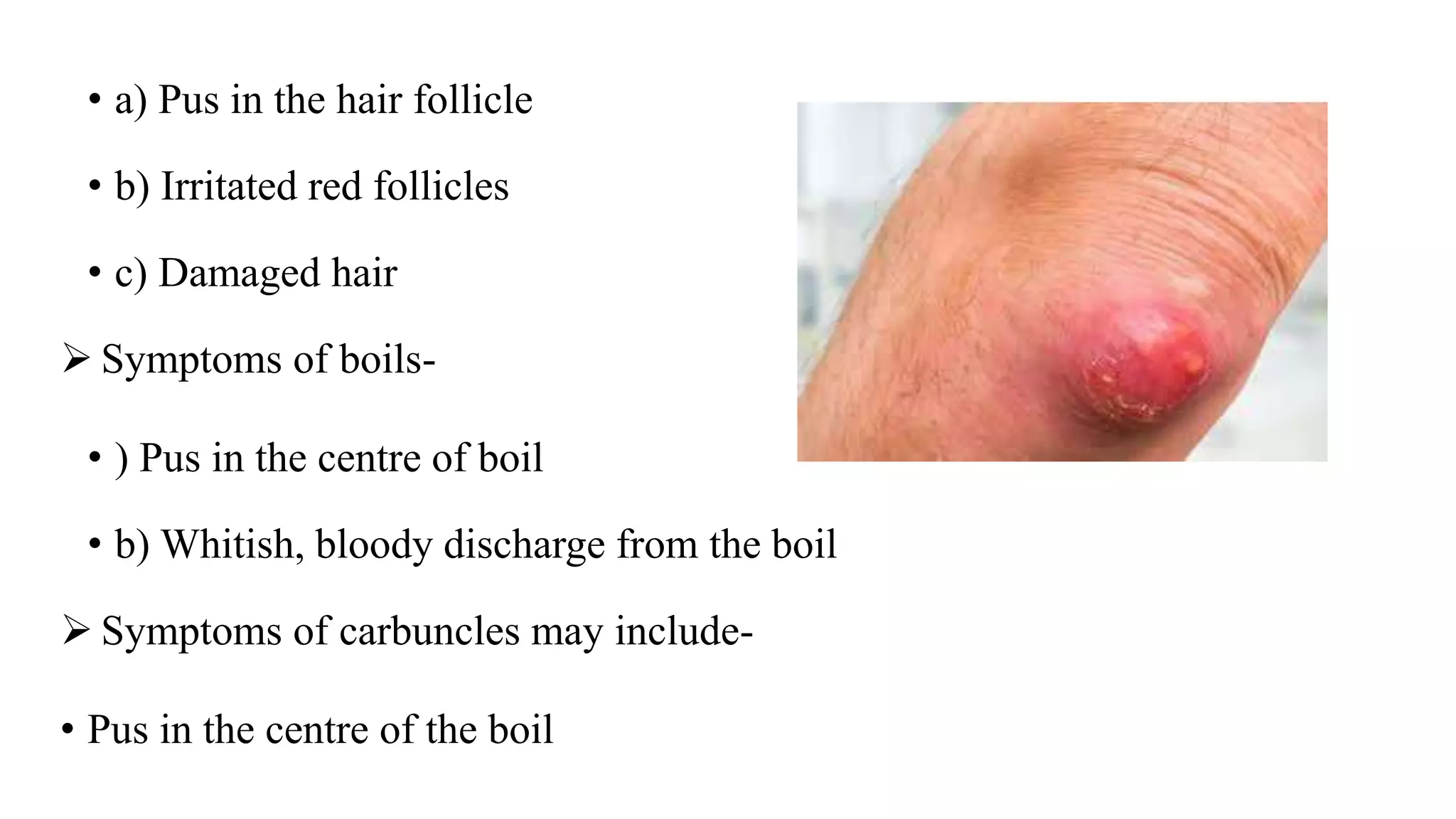
Pyoderma and bacterial skin infections can take several forms including impetigo, cellulitis, folliculitis, boils, and carbuncles. Impetigo is a superficial infection caused by Streptococcus or Staphylococcus that presents as crusty lesions that are contagious. Cellulitis is a deep bacterial skin infection commonly caused by Streptococcus or Staphylococcus that presents as swollen, warm, painful skin with red streaks and fever. Staphylococcal scalded skin syndrome causes skin reddening and blistering that gives the skin a burned appearance and is usually not life-threatening in children.