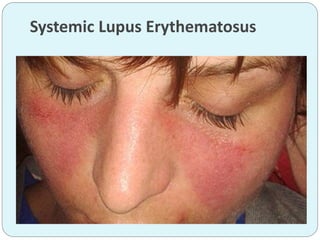
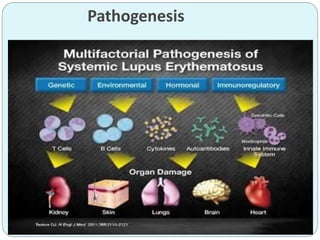
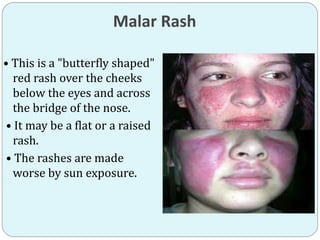
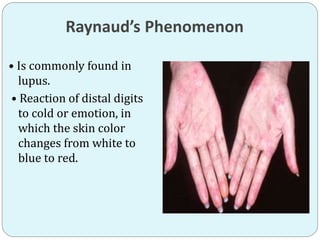
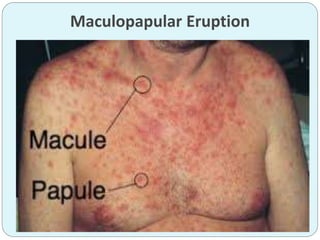
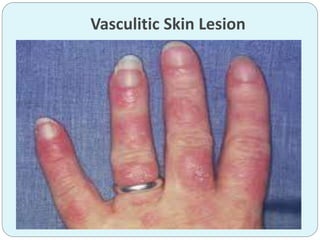
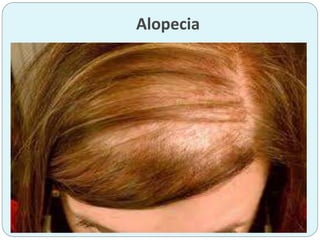
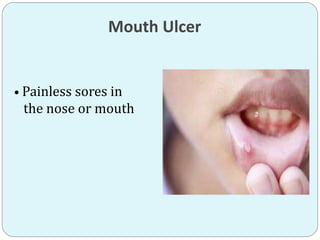
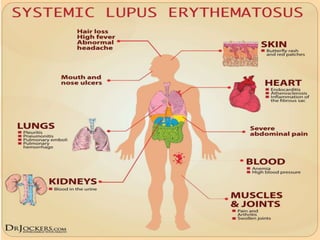
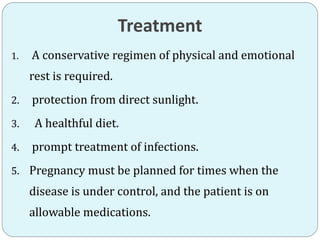
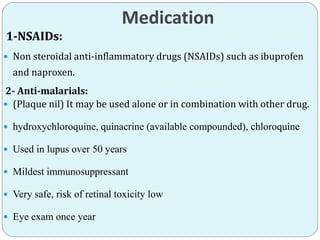
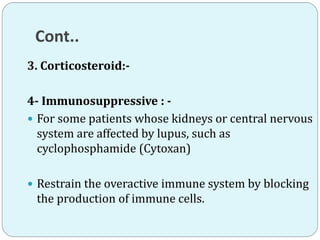
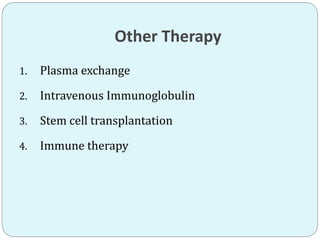
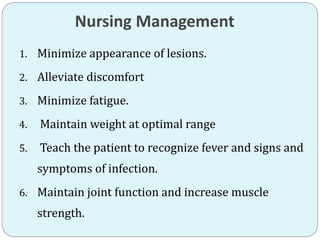
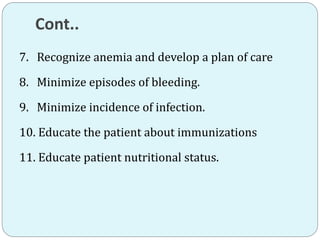
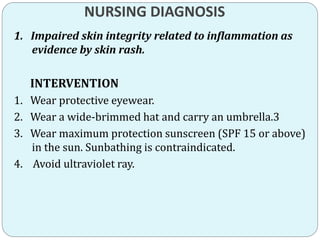
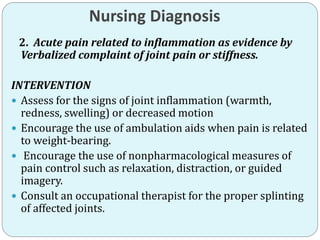
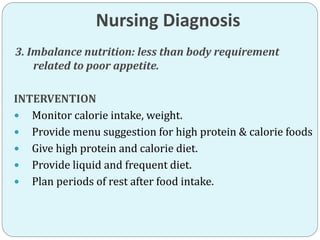
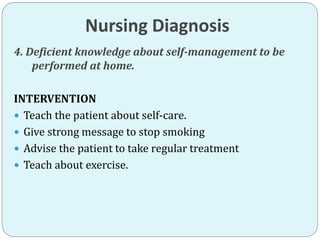
Systemic lupus erythematosus is an autoimmune disease where the immune system attacks healthy cells and tissues. It most commonly affects women between 15-40 years old. Symptoms include painful joints, rashes, fatigue, and organ inflammation. The cause is unknown but genetics and environmental factors like sunlight play a role. Treatment focuses on reducing inflammation with medications like NSAIDs, anti-malarials, and corticosteroids. Nursing care centers around managing symptoms, preventing infections and flares, maintaining nutrition, and educating patients on self-management.