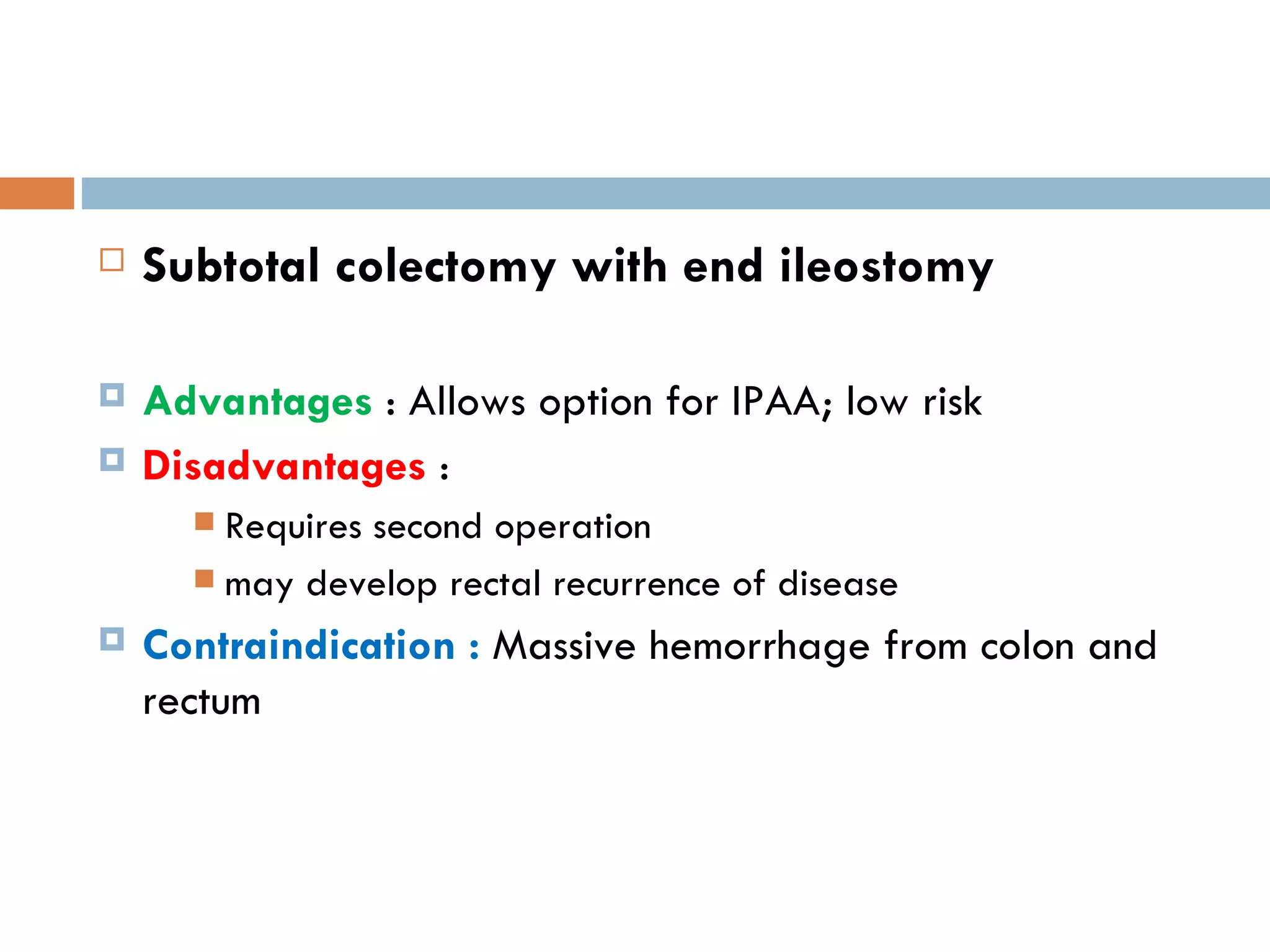
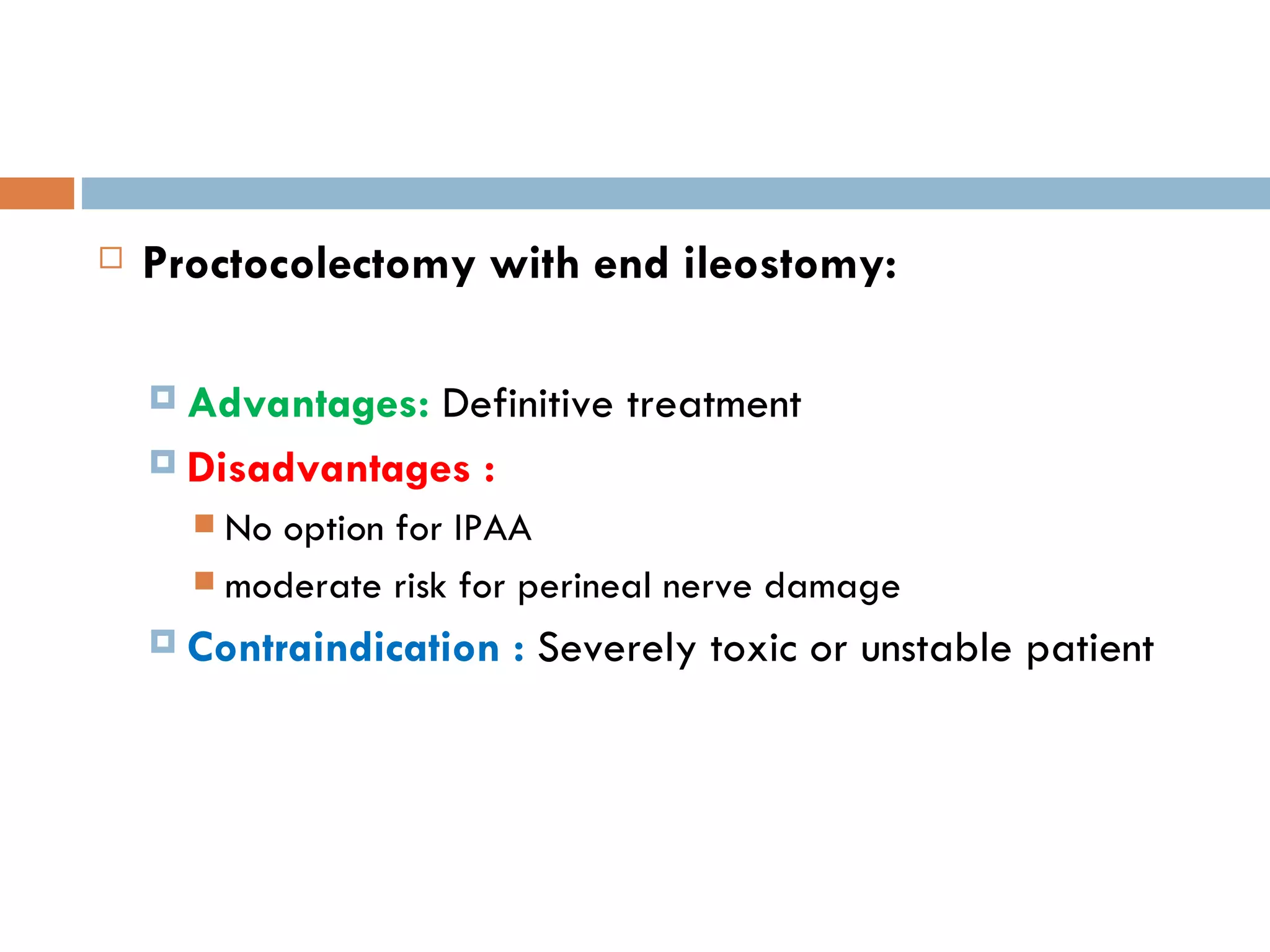
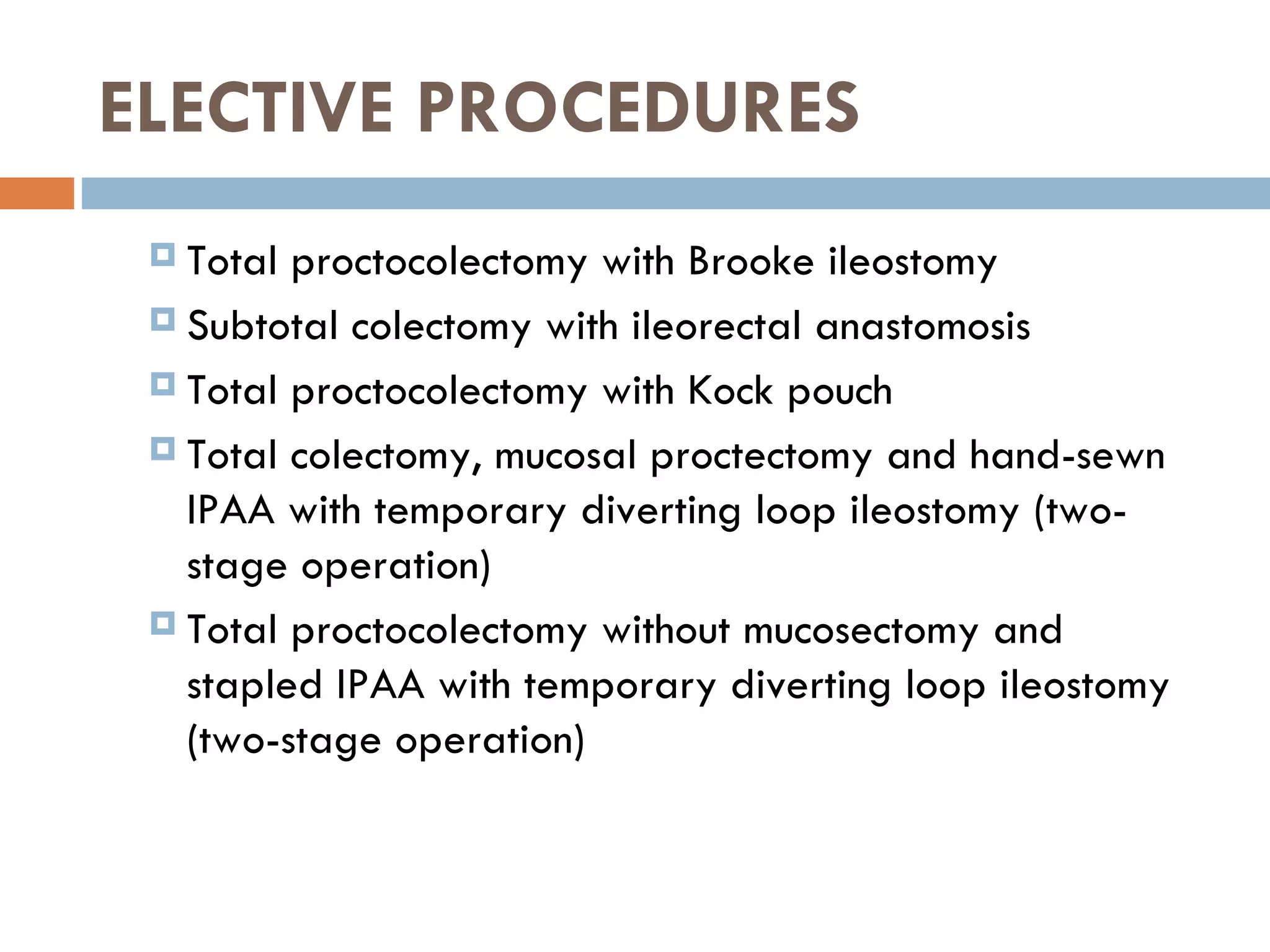
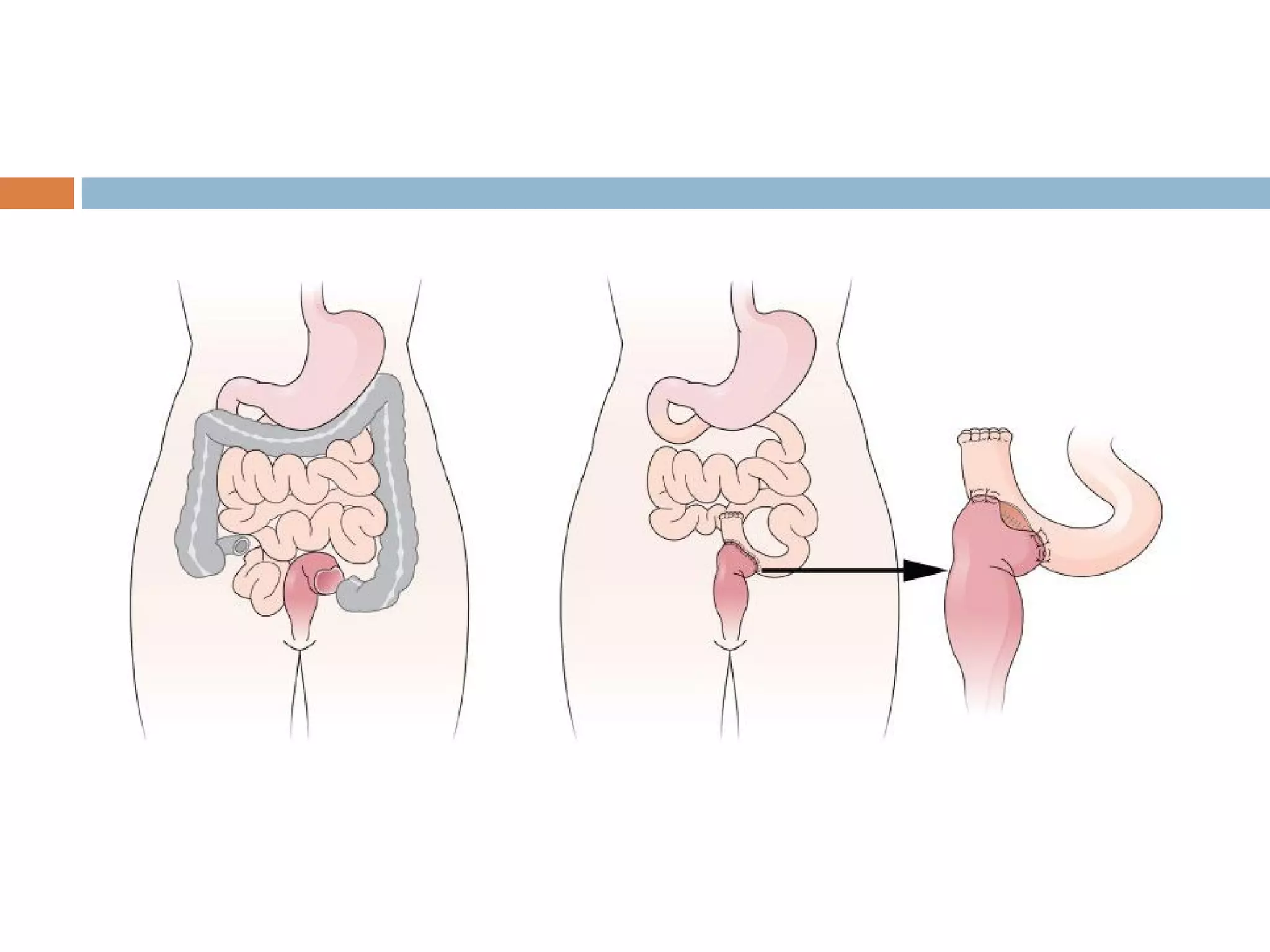
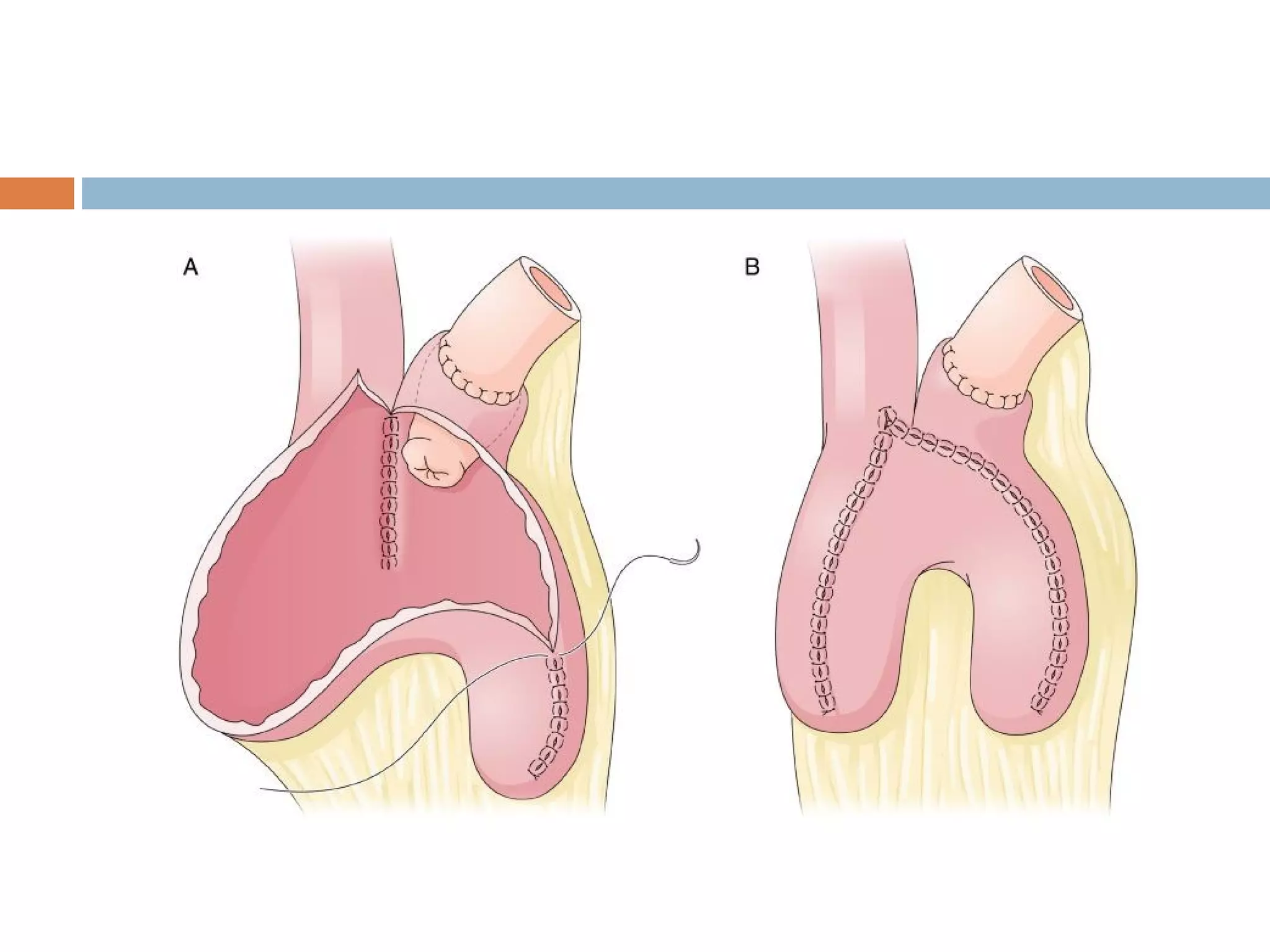
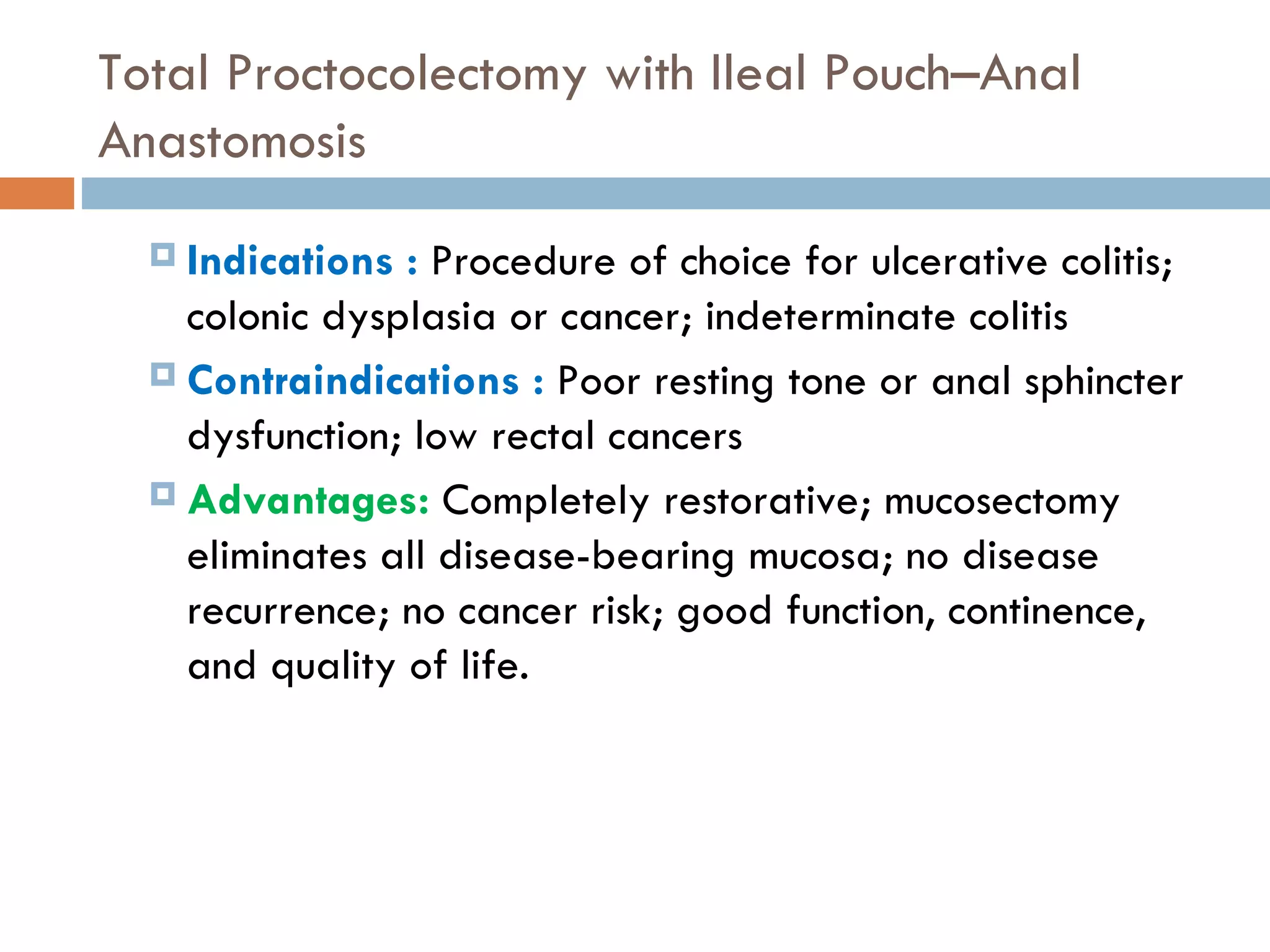
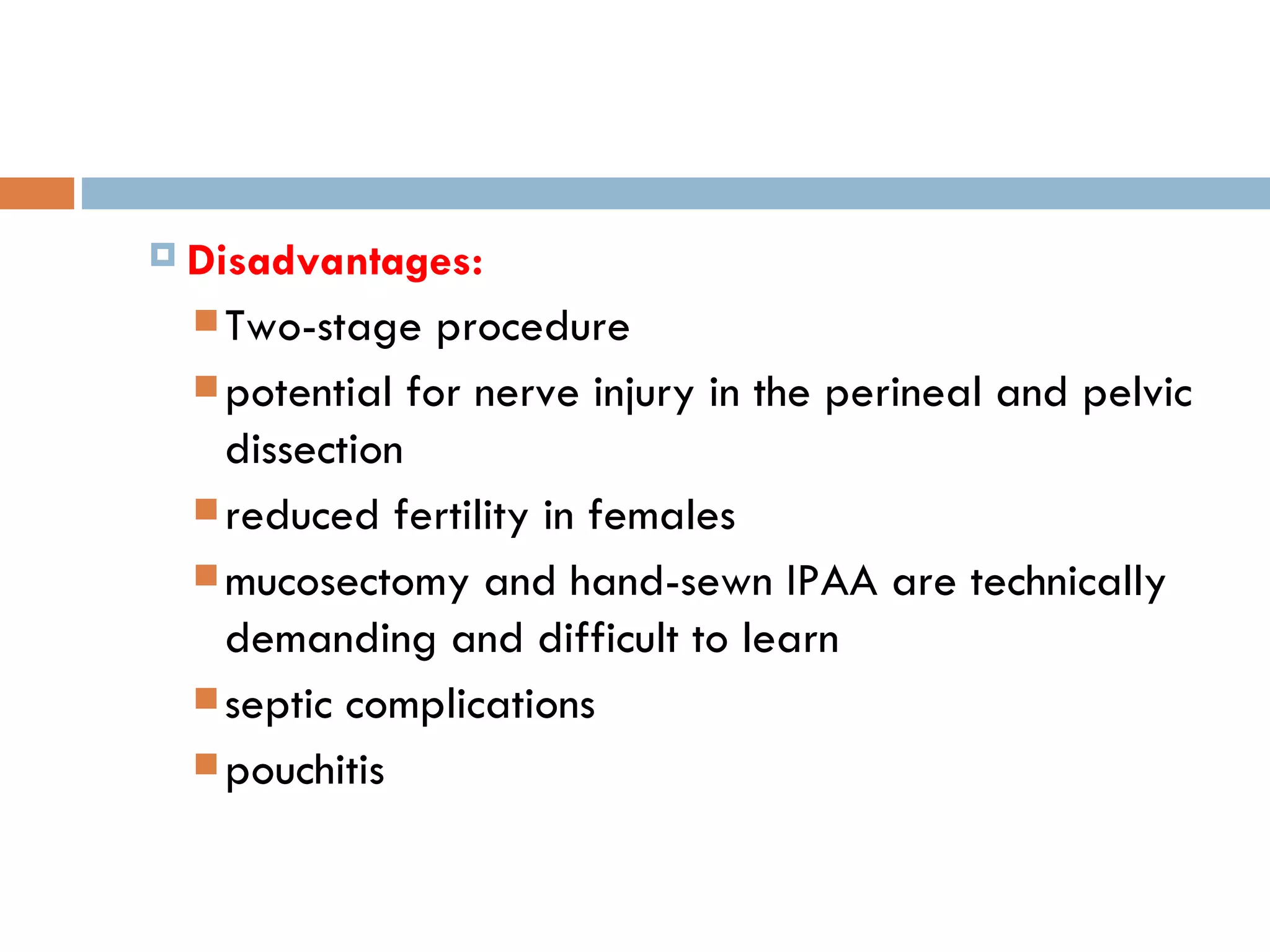
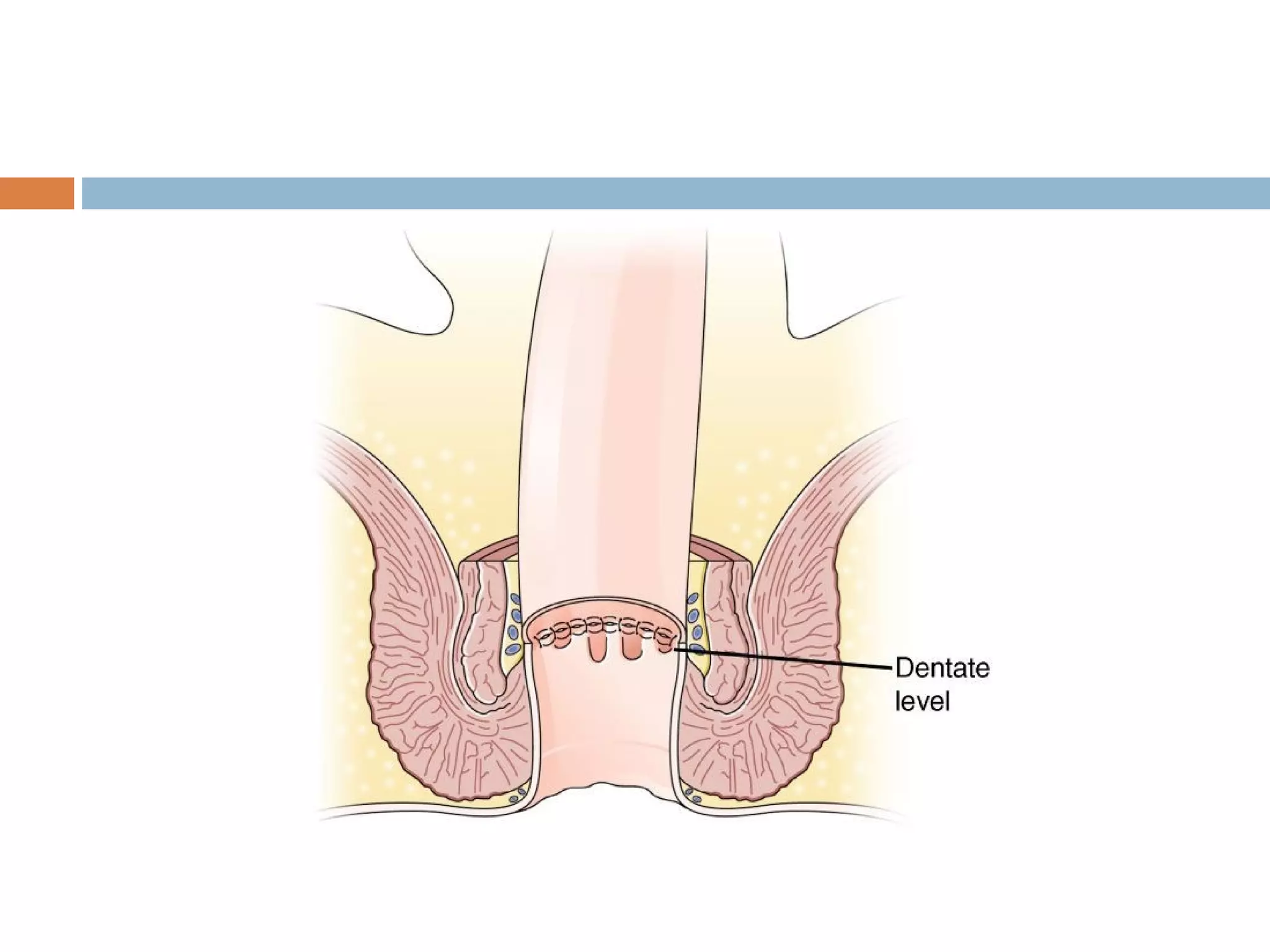
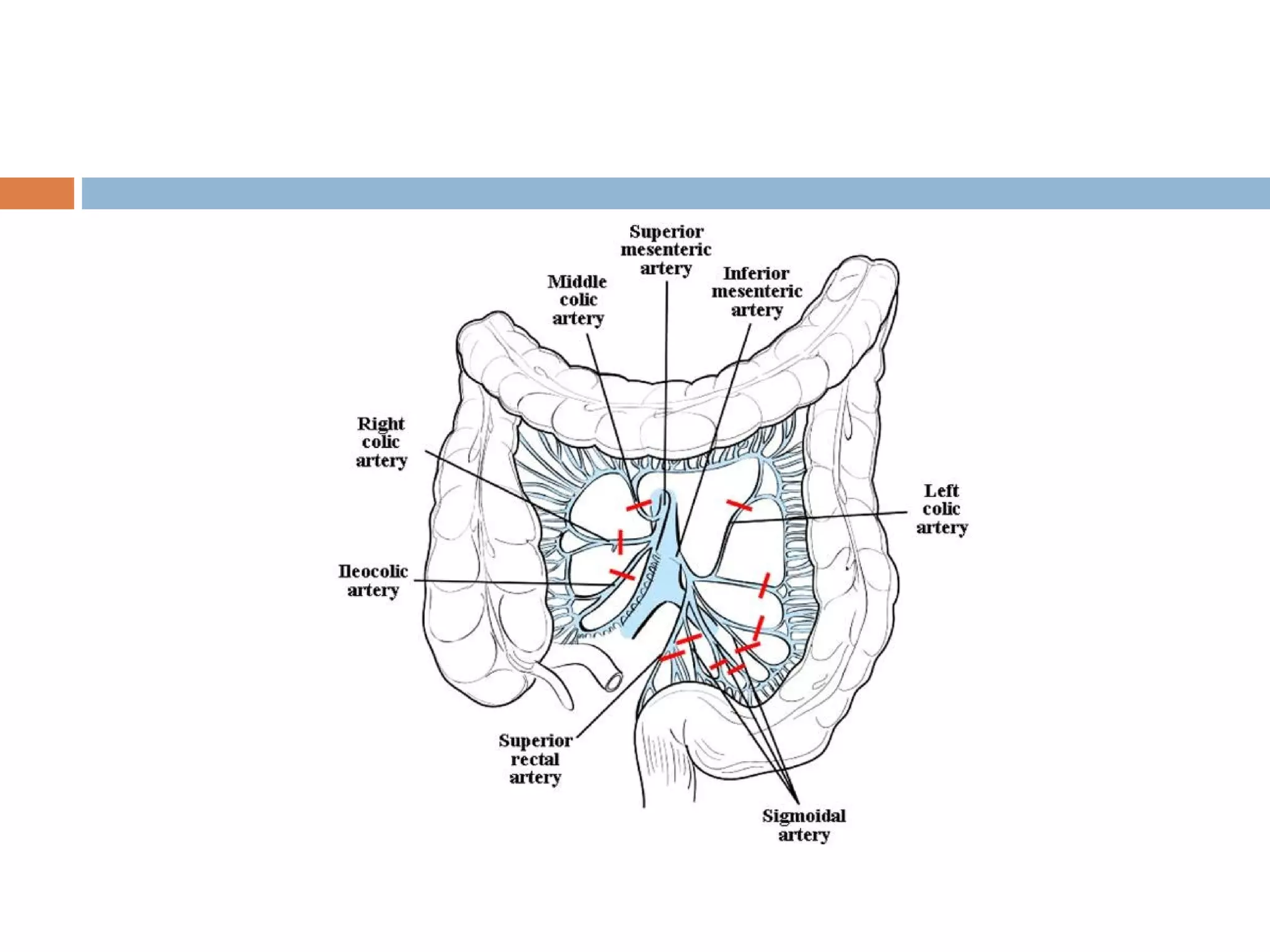
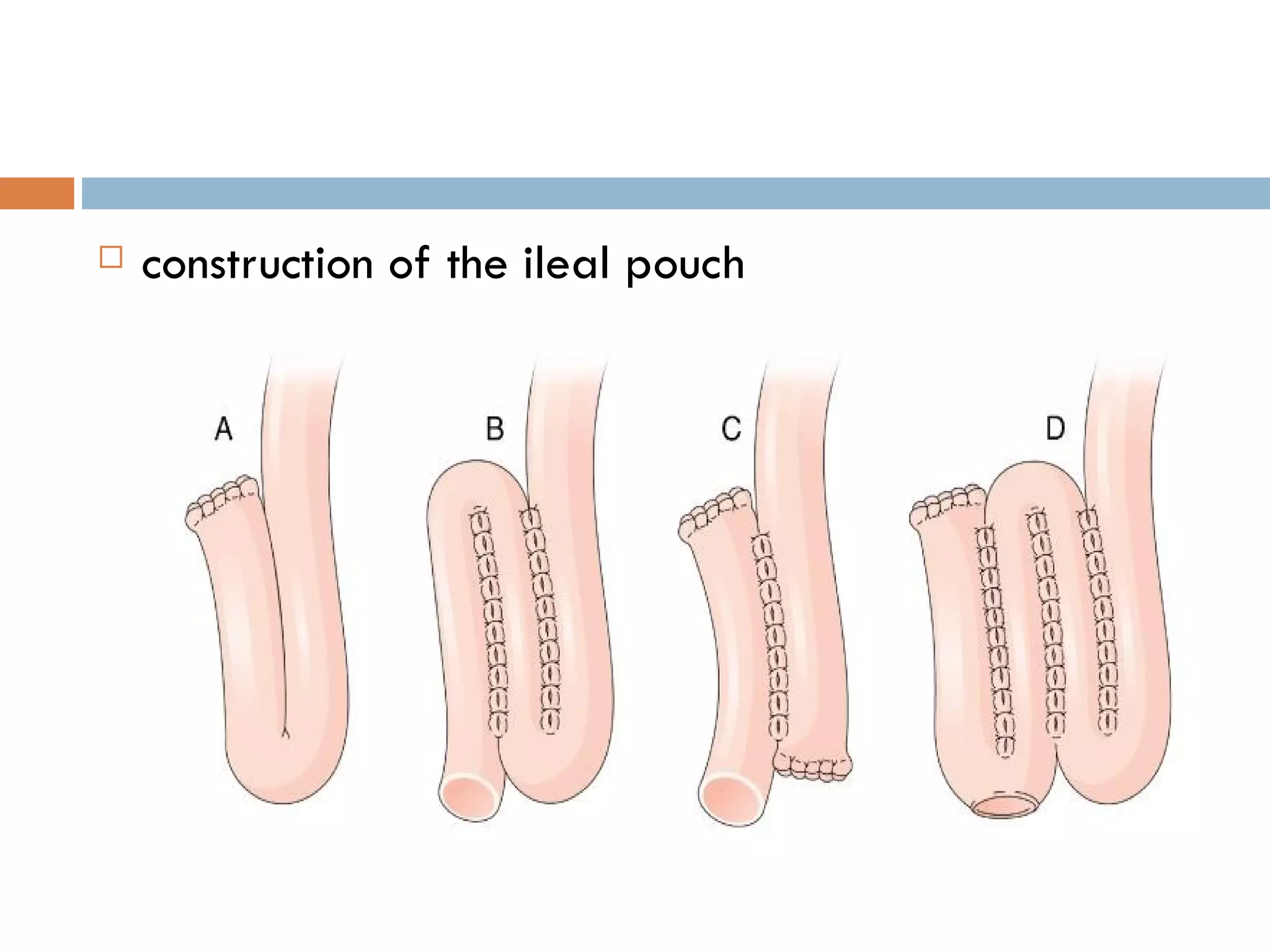
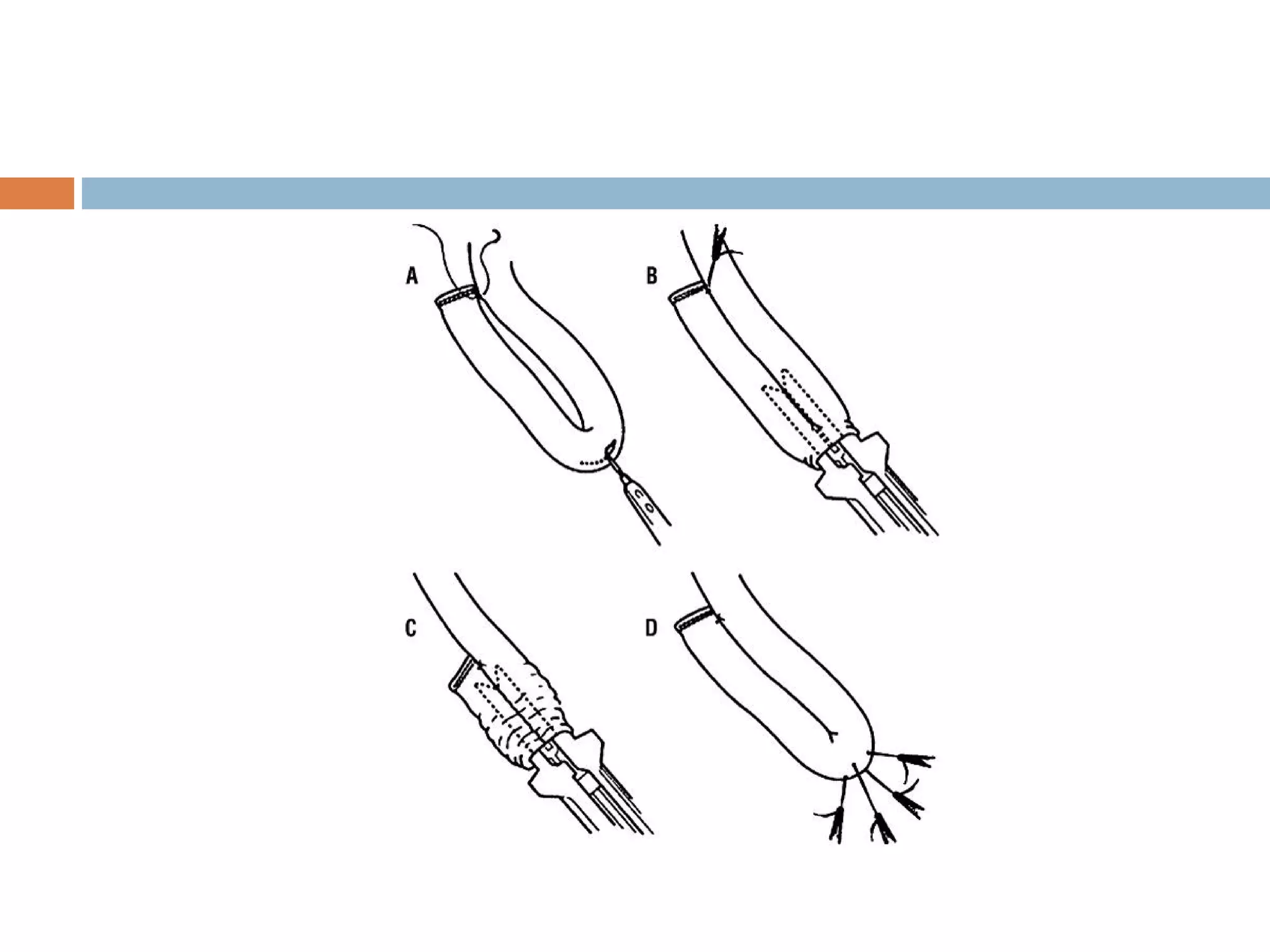
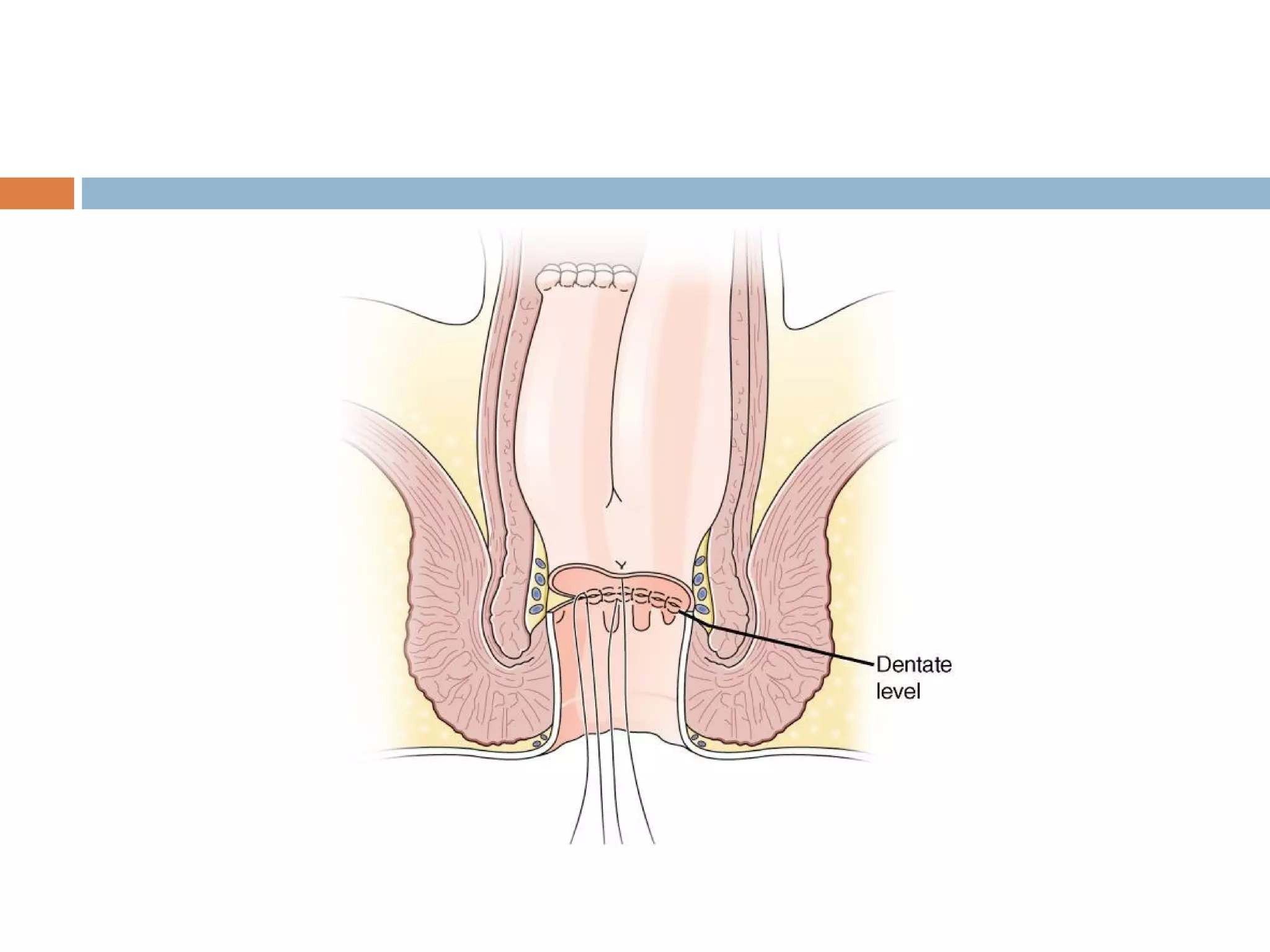
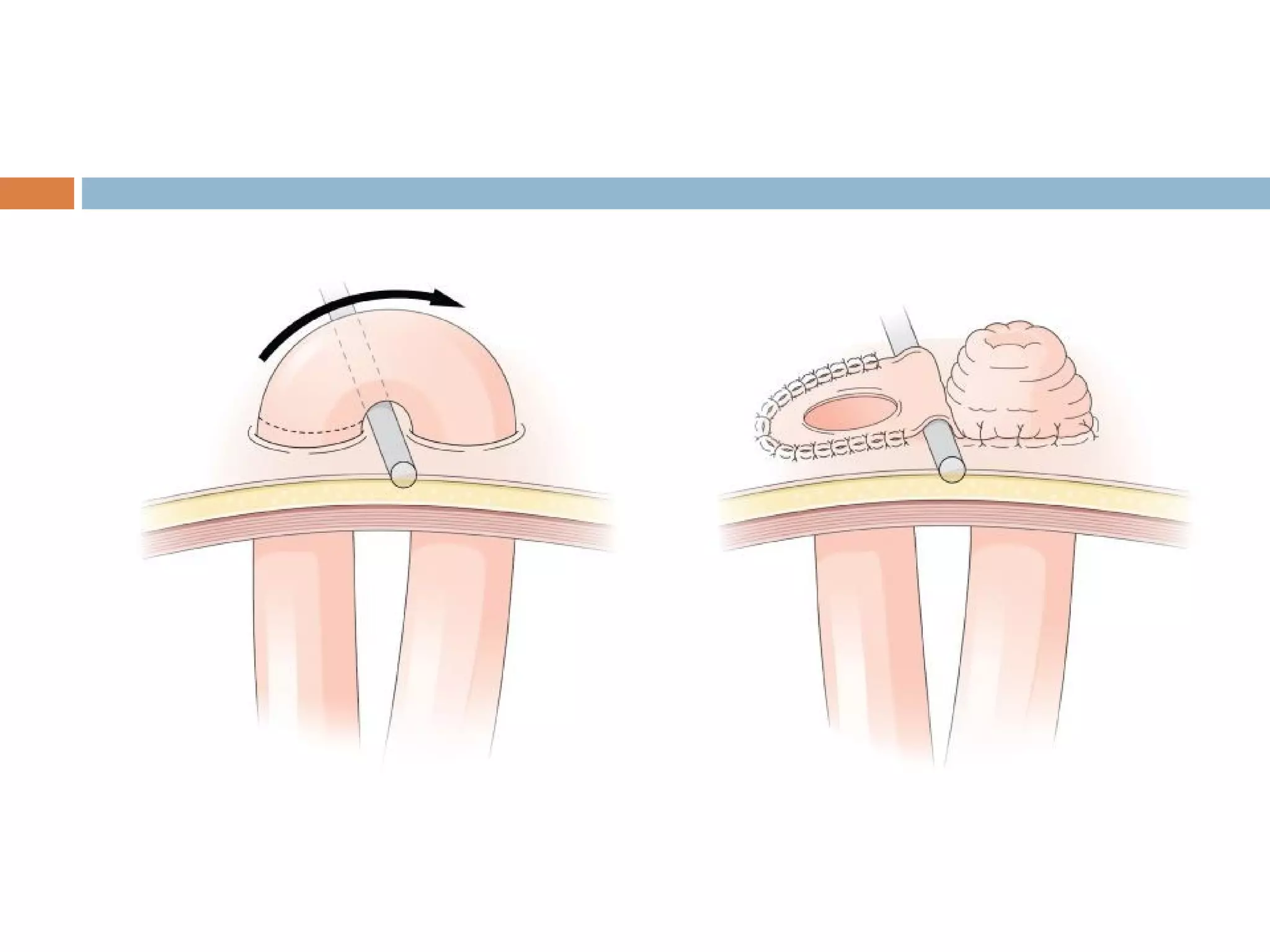
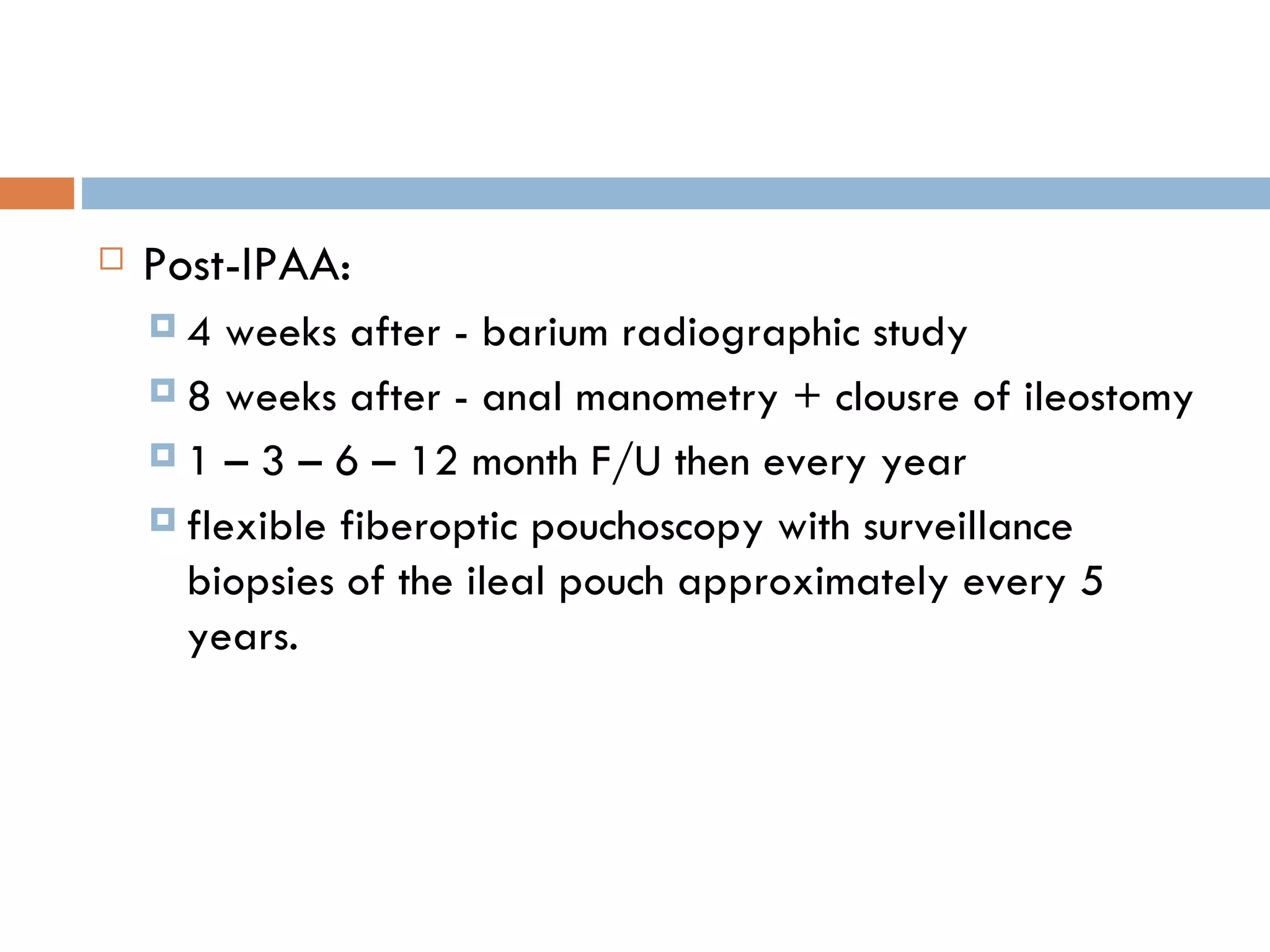
Surgical management of ulcerative colitis includes both emergency and elective procedures. Emergency surgeries are indicated for complications like toxic megacolon or hemorrhage. Elective surgeries are considered for intractable disease or risk factors like dysplasia. Common procedures include subtotal colectomy, proctocolectomy with Brooke ileostomy, and restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA). The IPAA aims to restore continence but has risks of complications like pouchitis or rarely Crohn's disease developing in the pouch. Long term surveillance after surgery is important to monitor for issues.