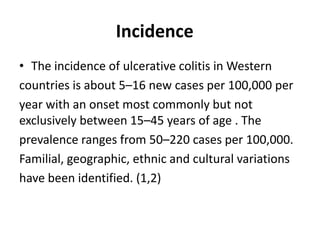
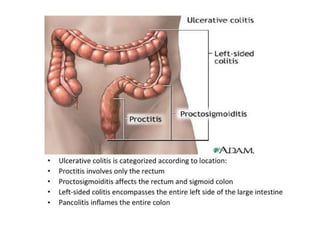
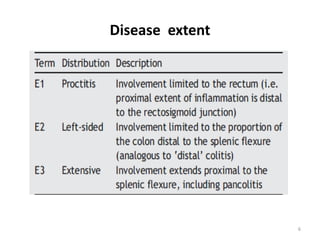
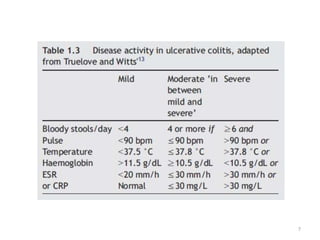
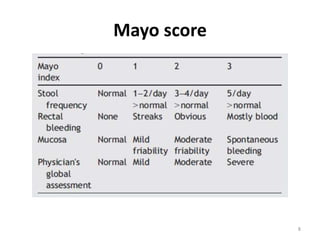
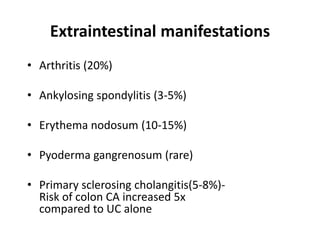
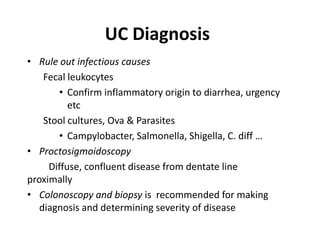
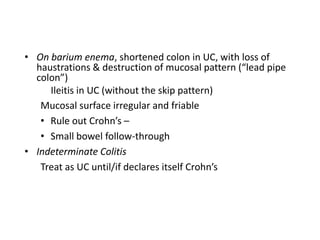
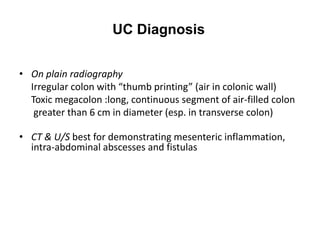
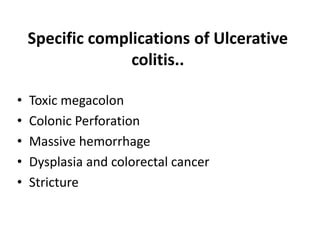
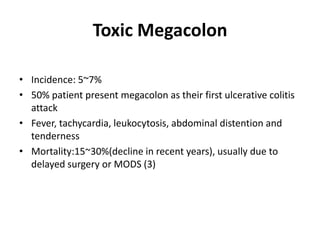
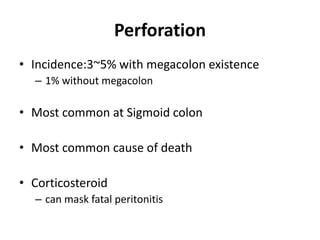
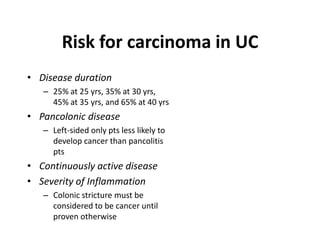
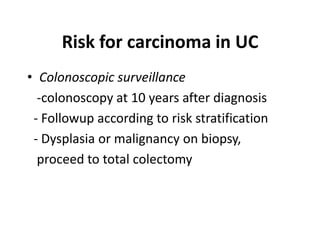
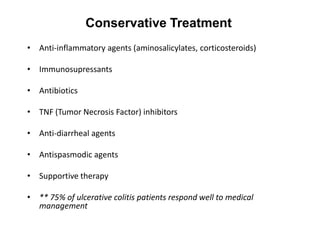
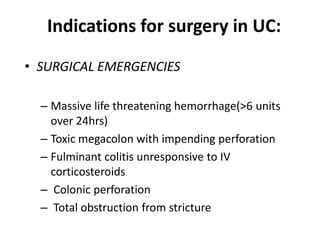
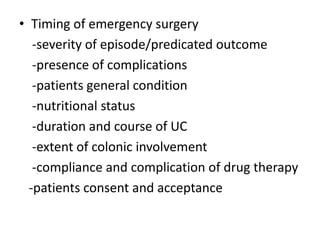
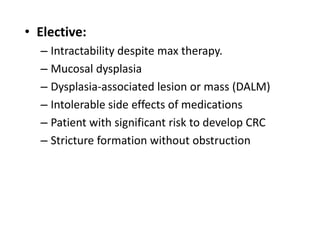
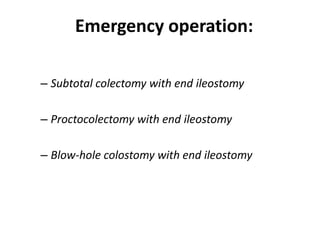
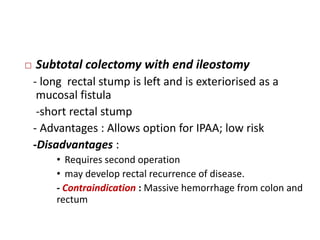
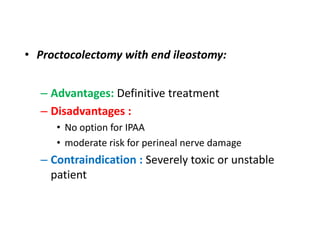
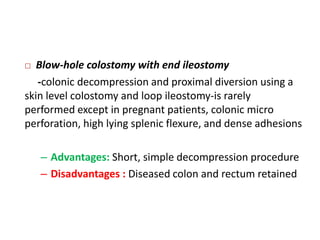
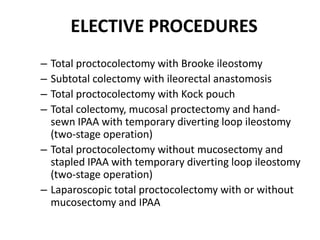
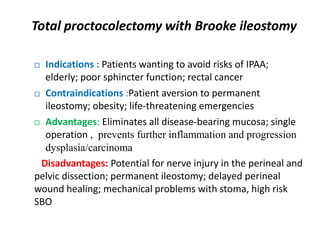
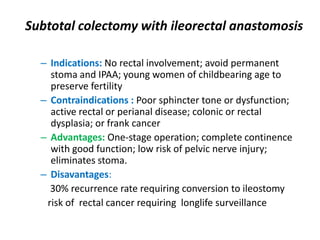
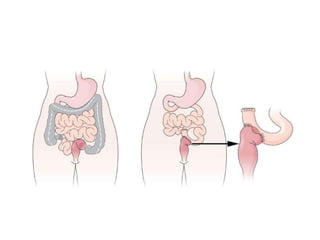
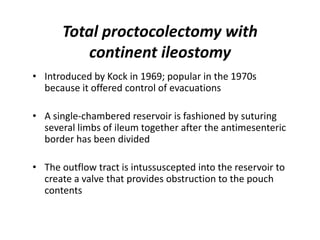
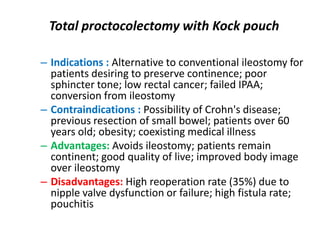
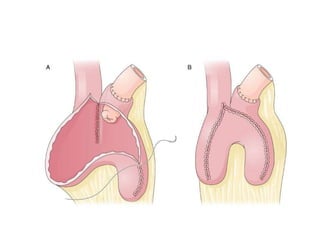
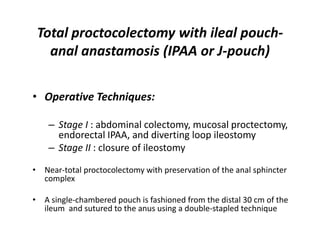
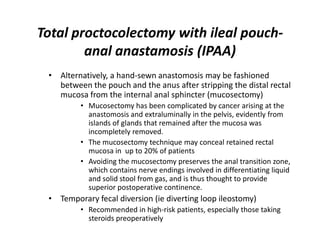
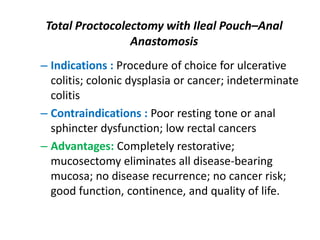
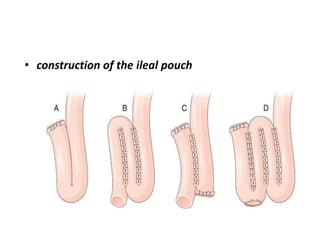
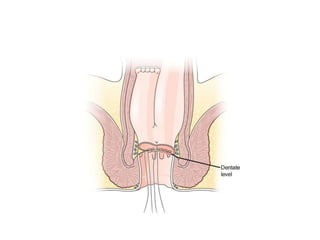
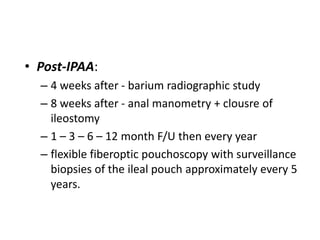
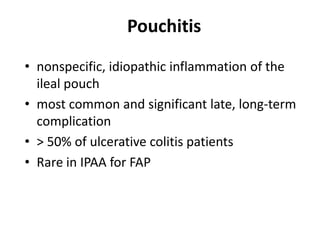
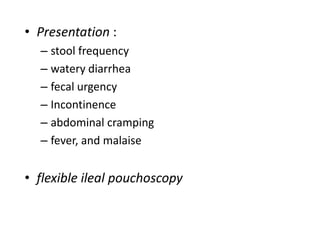
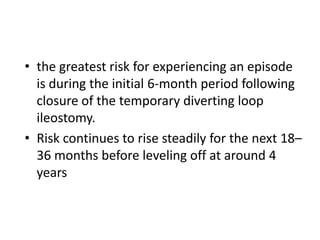
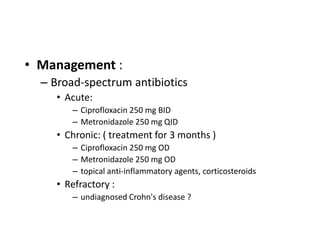
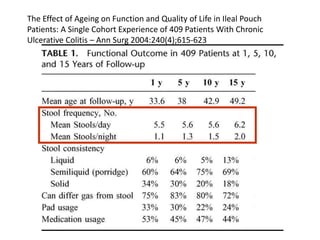
Ulcerative colitis is a chronic inflammatory bowel disease that causes continuous inflammation of the colon without granuloma formation. It commonly has an onset between ages 15-45 and is characterized by relapsing and remitting symptoms. Diagnosis involves ruling out infections and confirming inflammatory changes in the colon through endoscopy and biopsy. Treatment focuses on medications to control inflammation, with surgery indicated for complications or treatment failure. Surgical options range from colectomy with ileostomy to total proctocolectomy with ileal pouch-anal anastomosis. Post-surgical complications can include pouchitis, Crohn's disease of the pouch, and dysplasia.