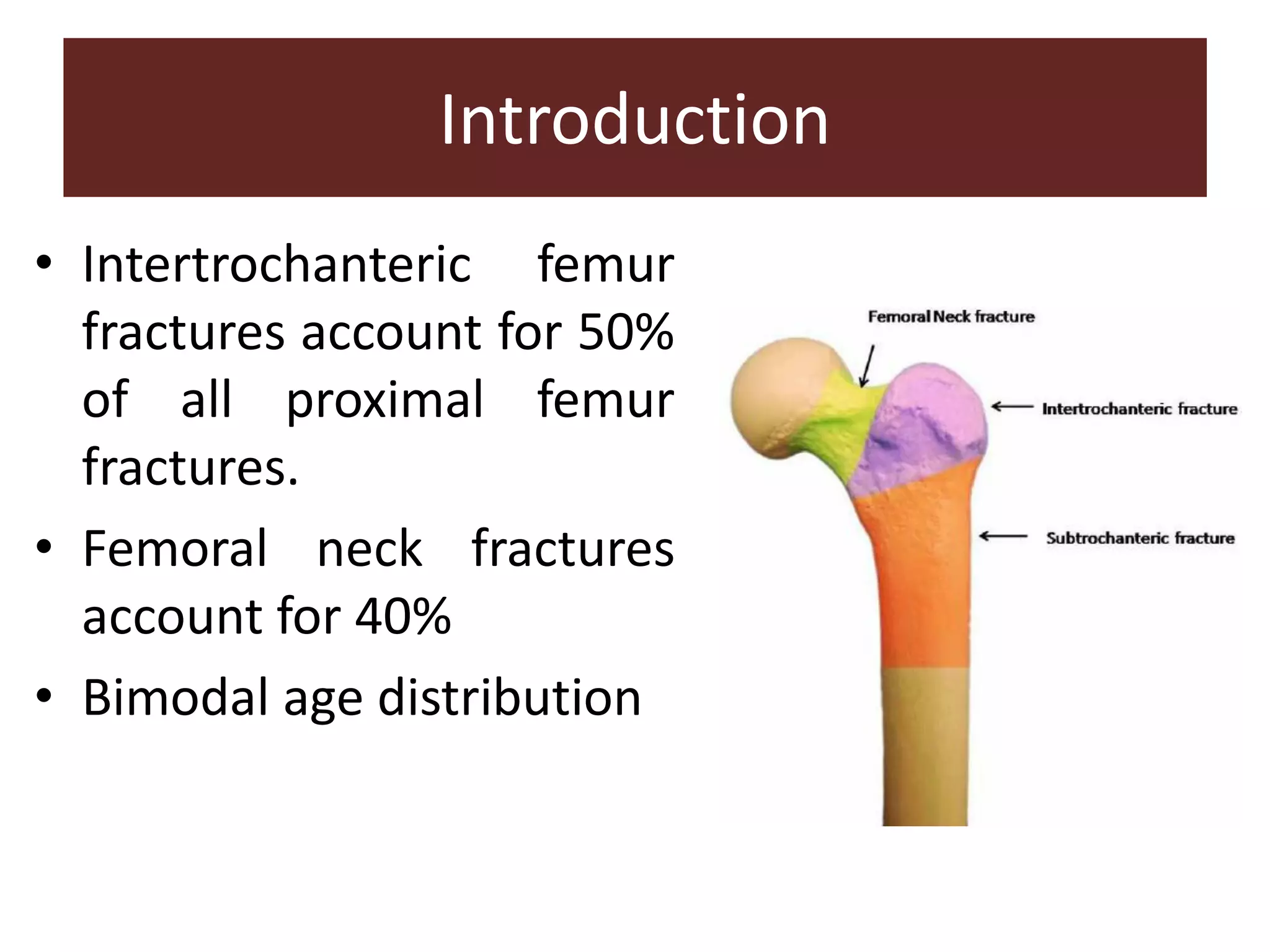
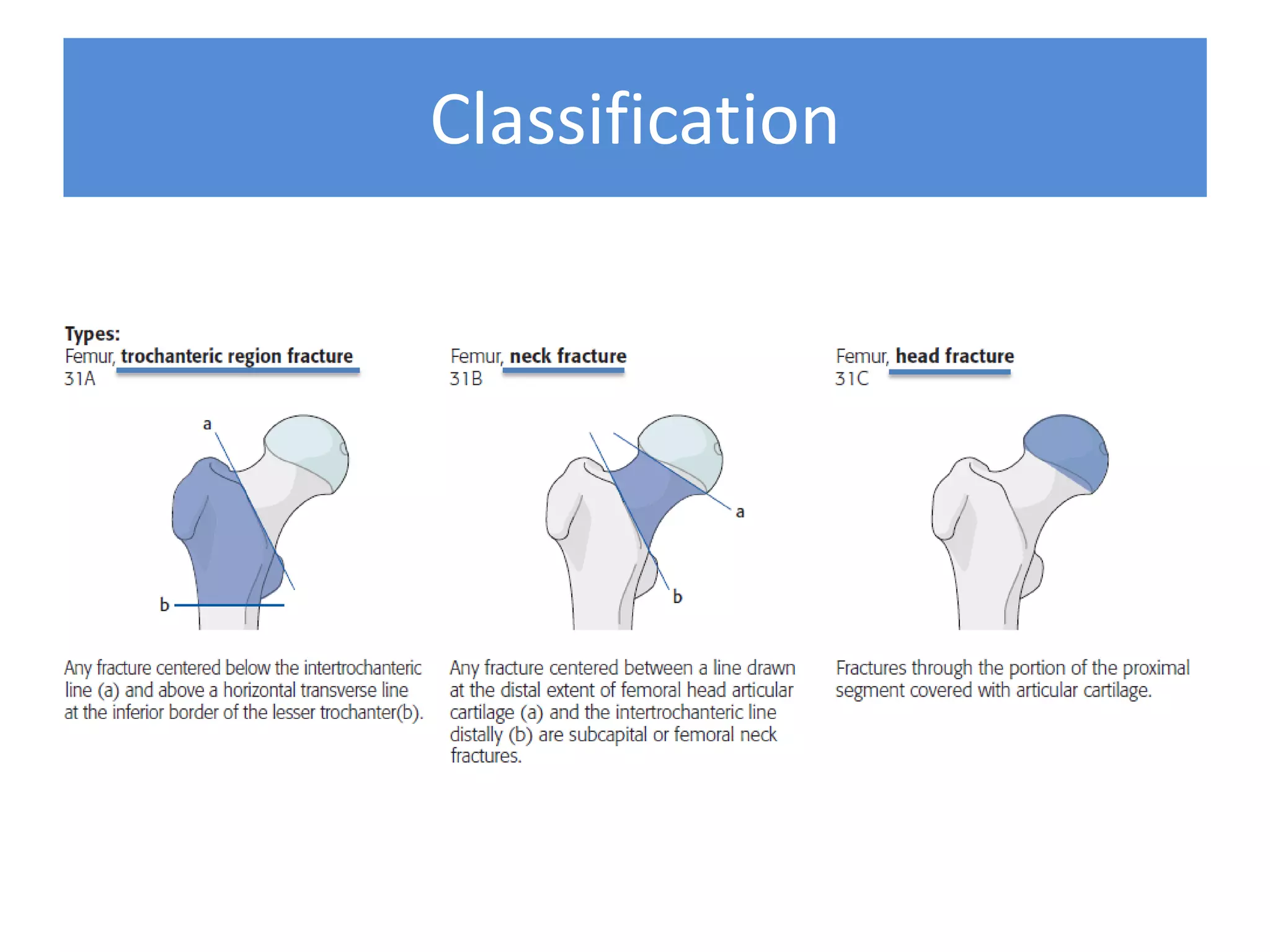
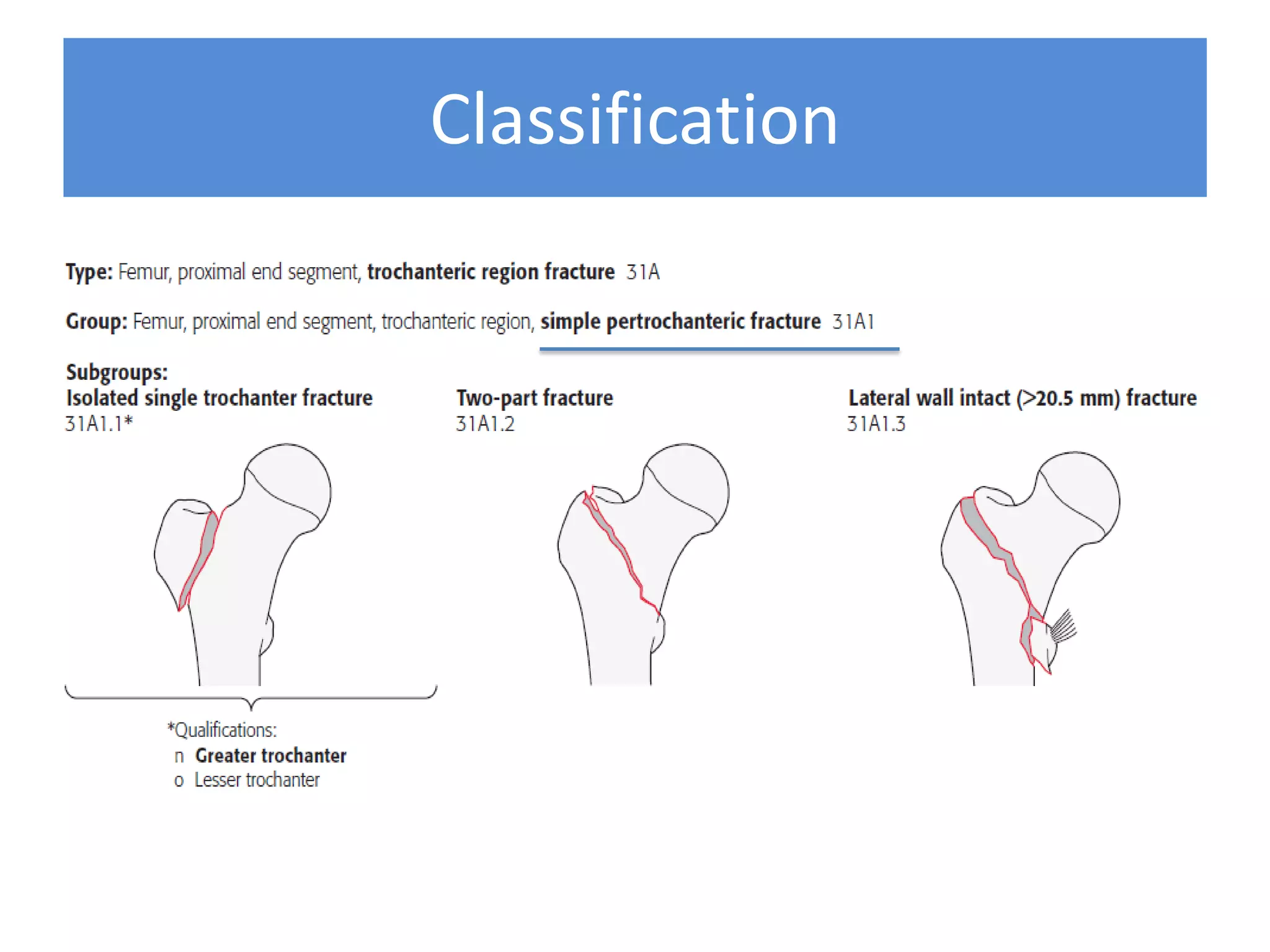
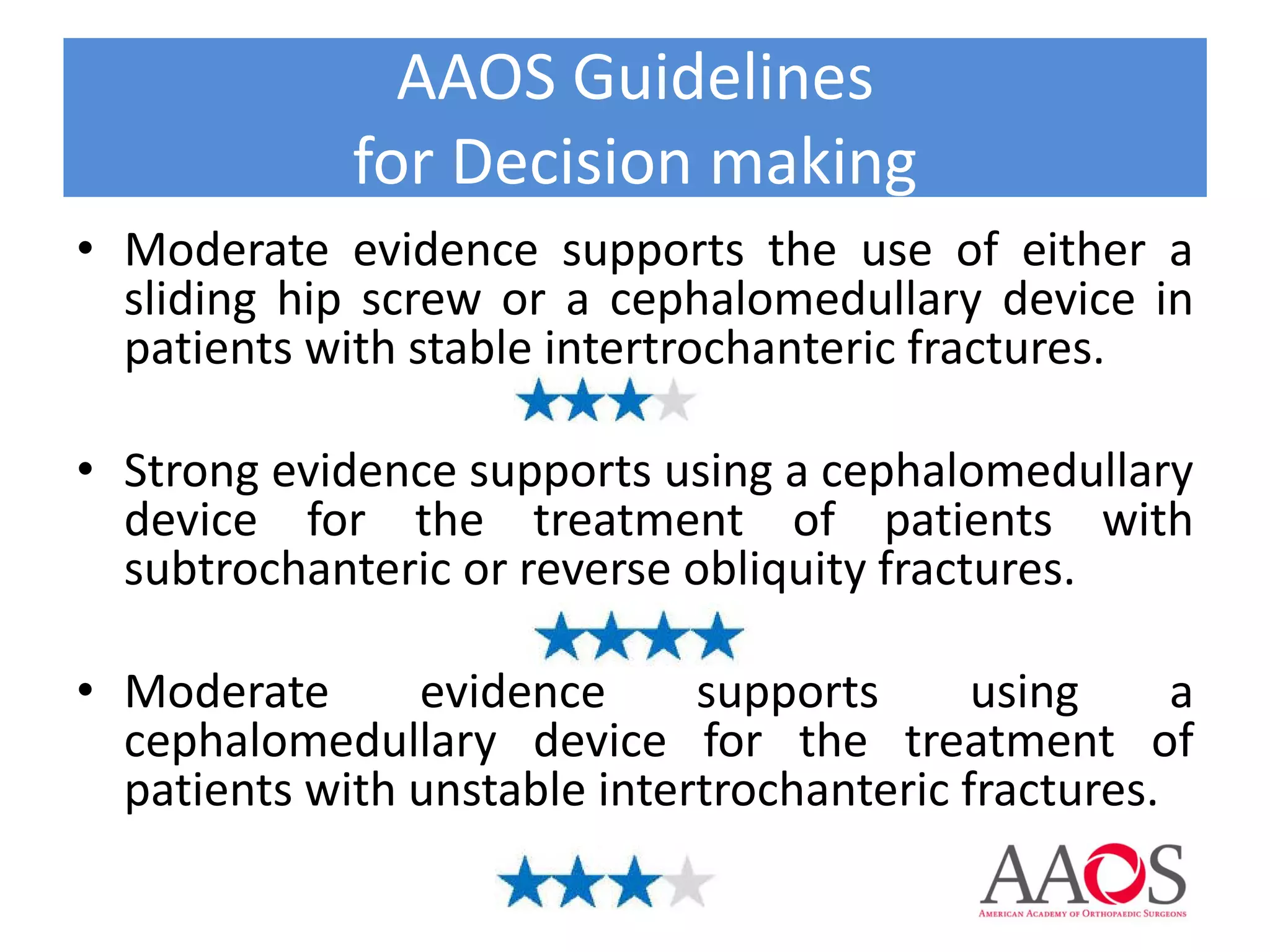
1) The document provides an evidence-based approach to treating proximal femoral fractures, including classification, decision making, preoperative planning, and postoperative care.
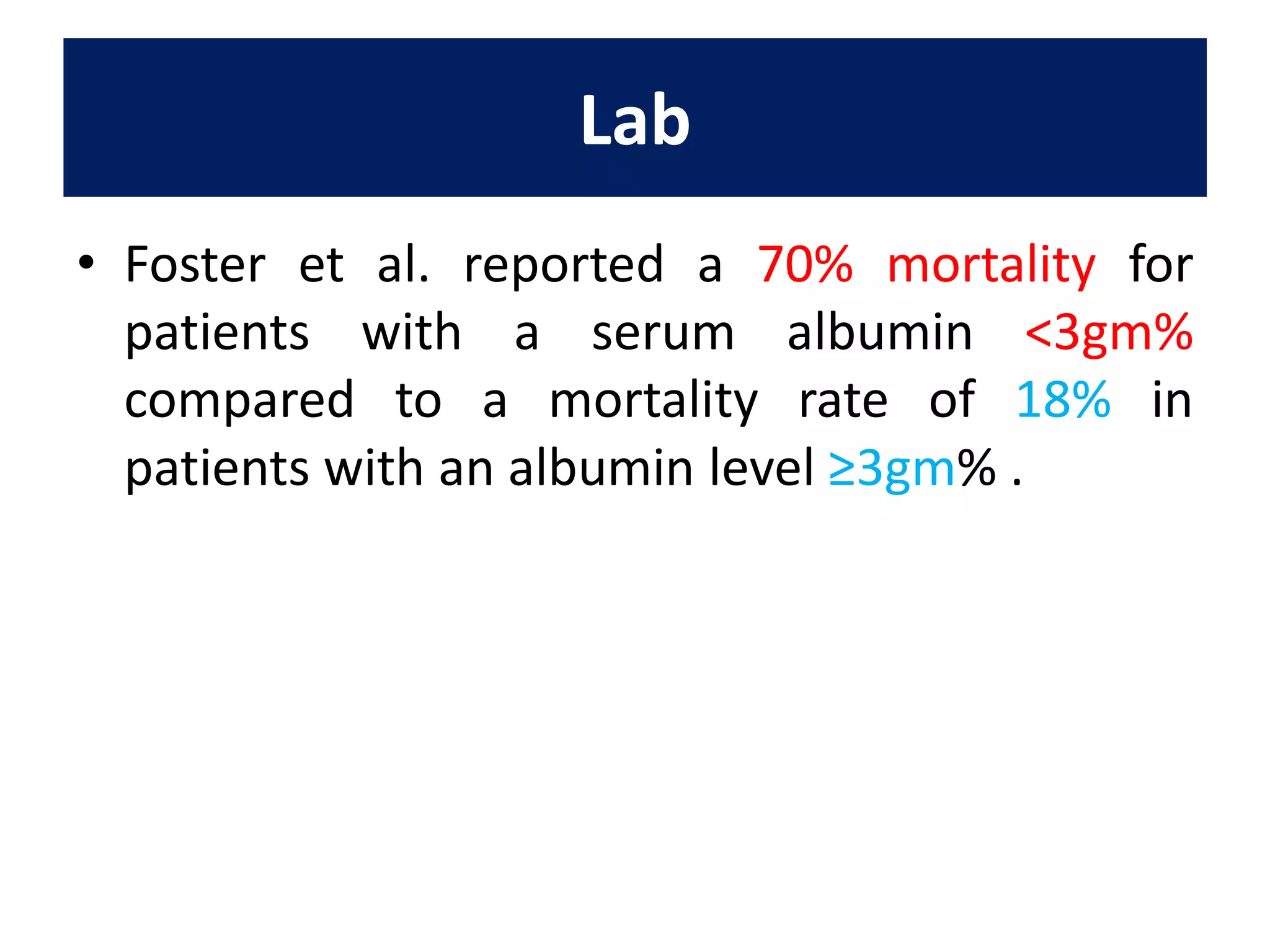
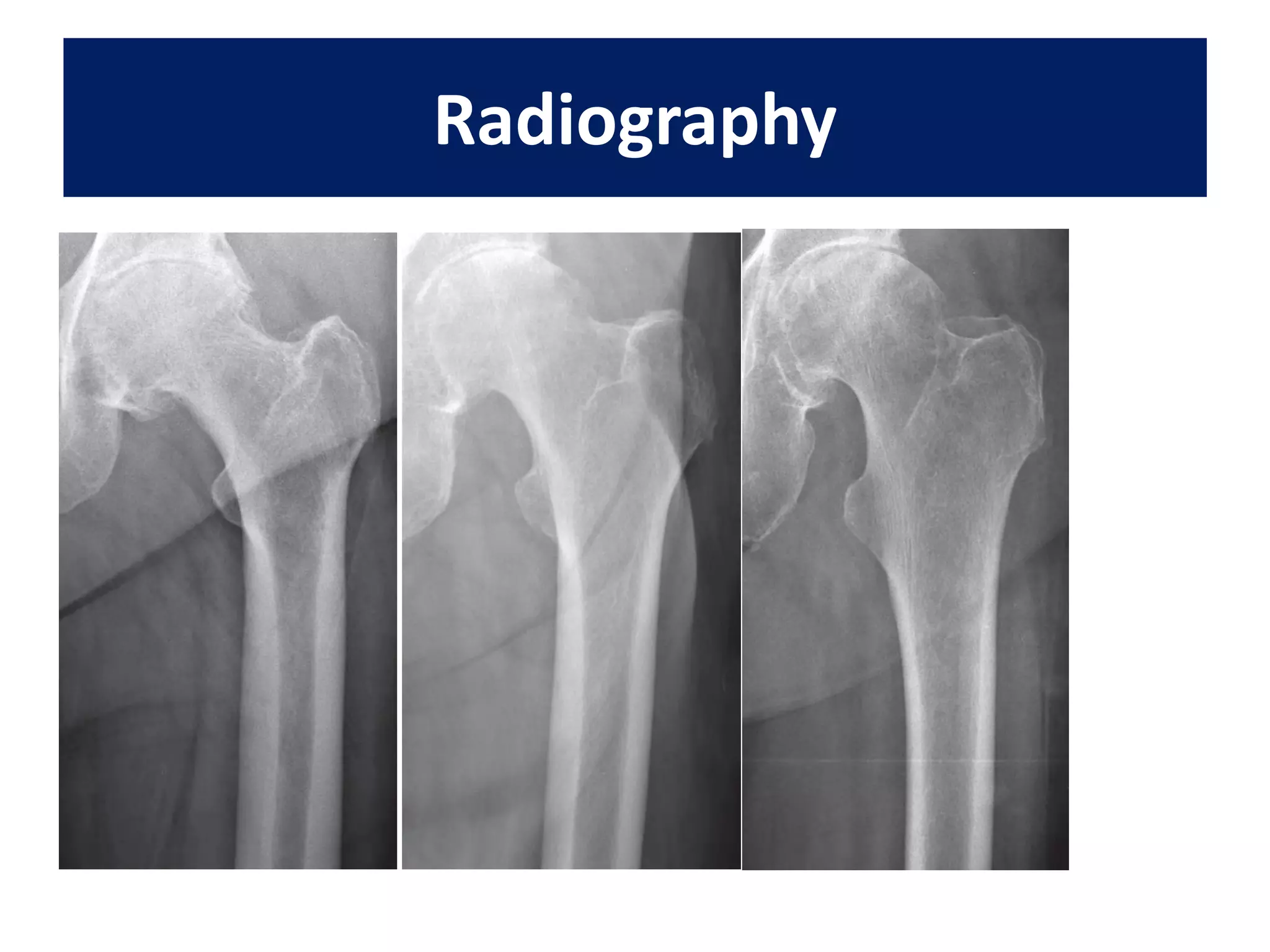
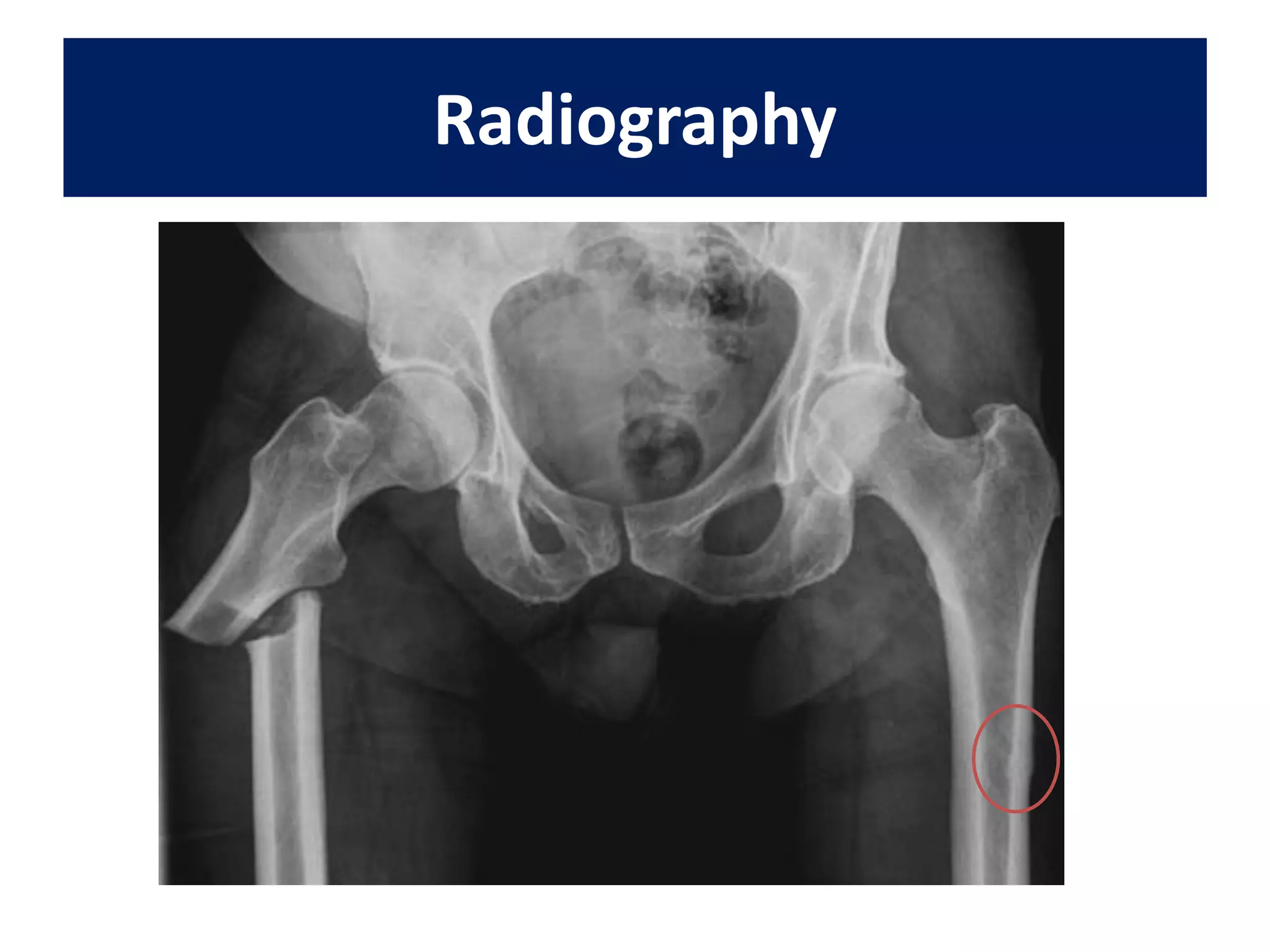
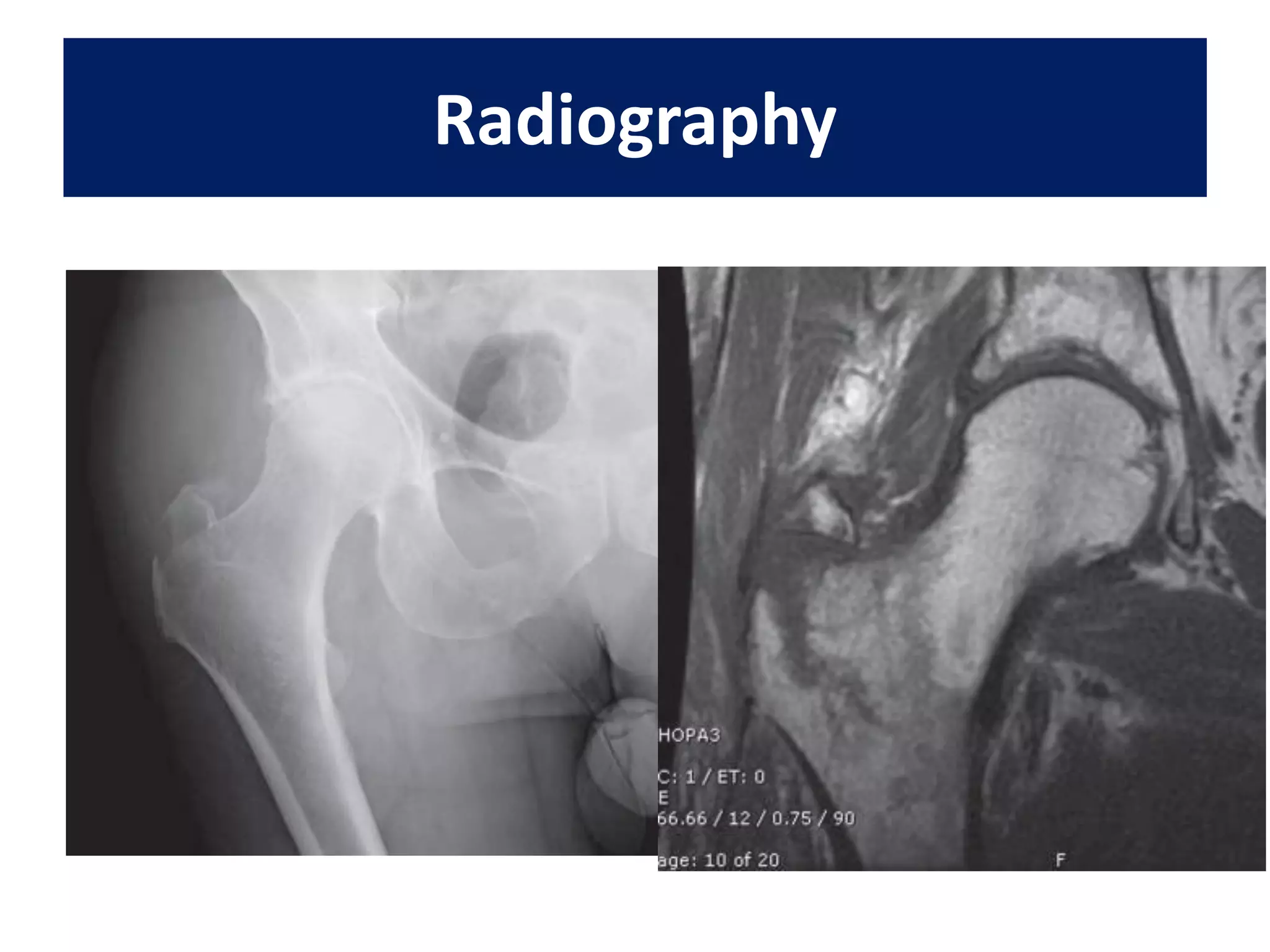
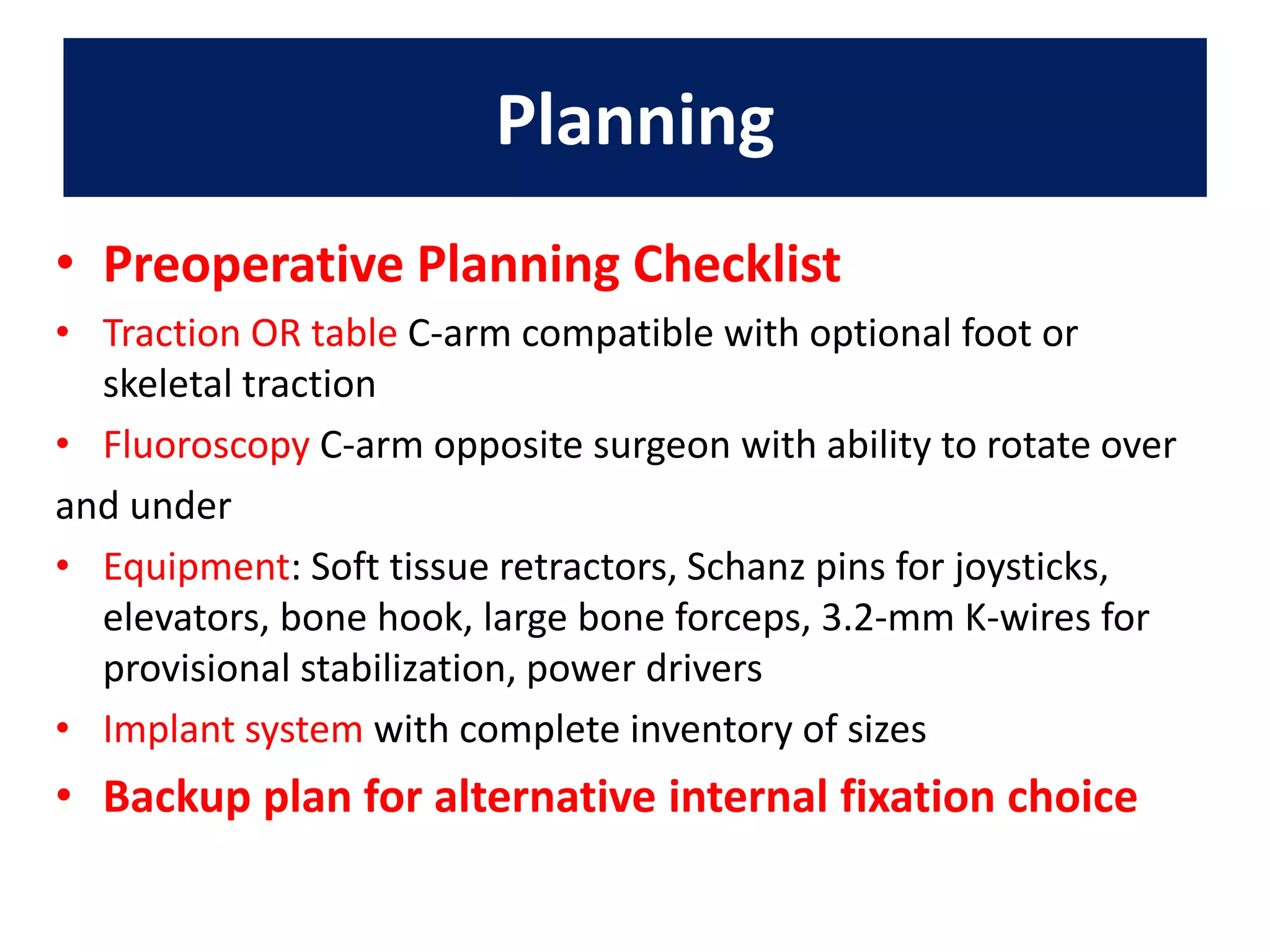
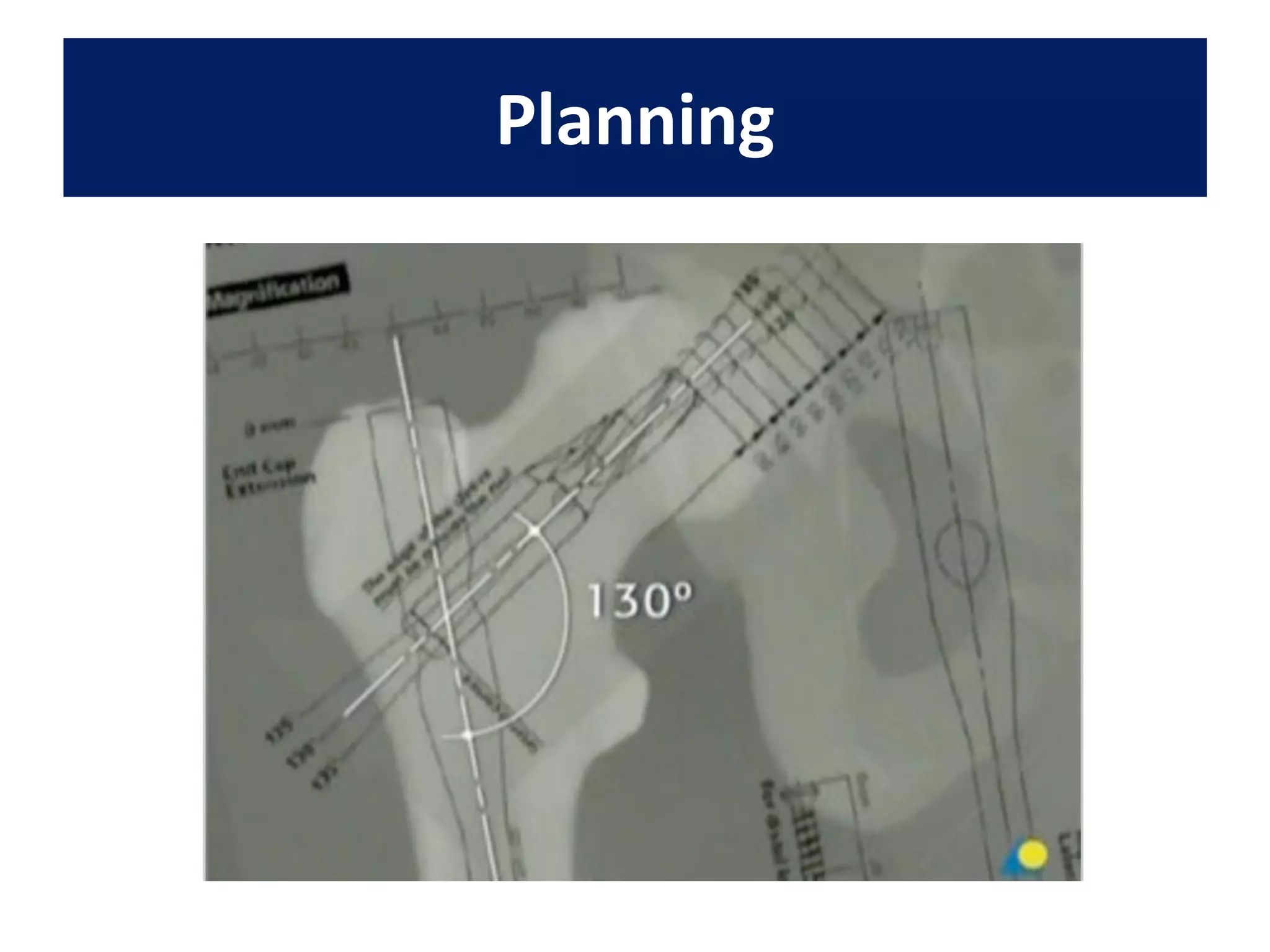
2) Key aspects of preoperative planning discussed include thorough patient history, physical exam, imaging including x-rays and MRI, and consideration of patient comorbidities.
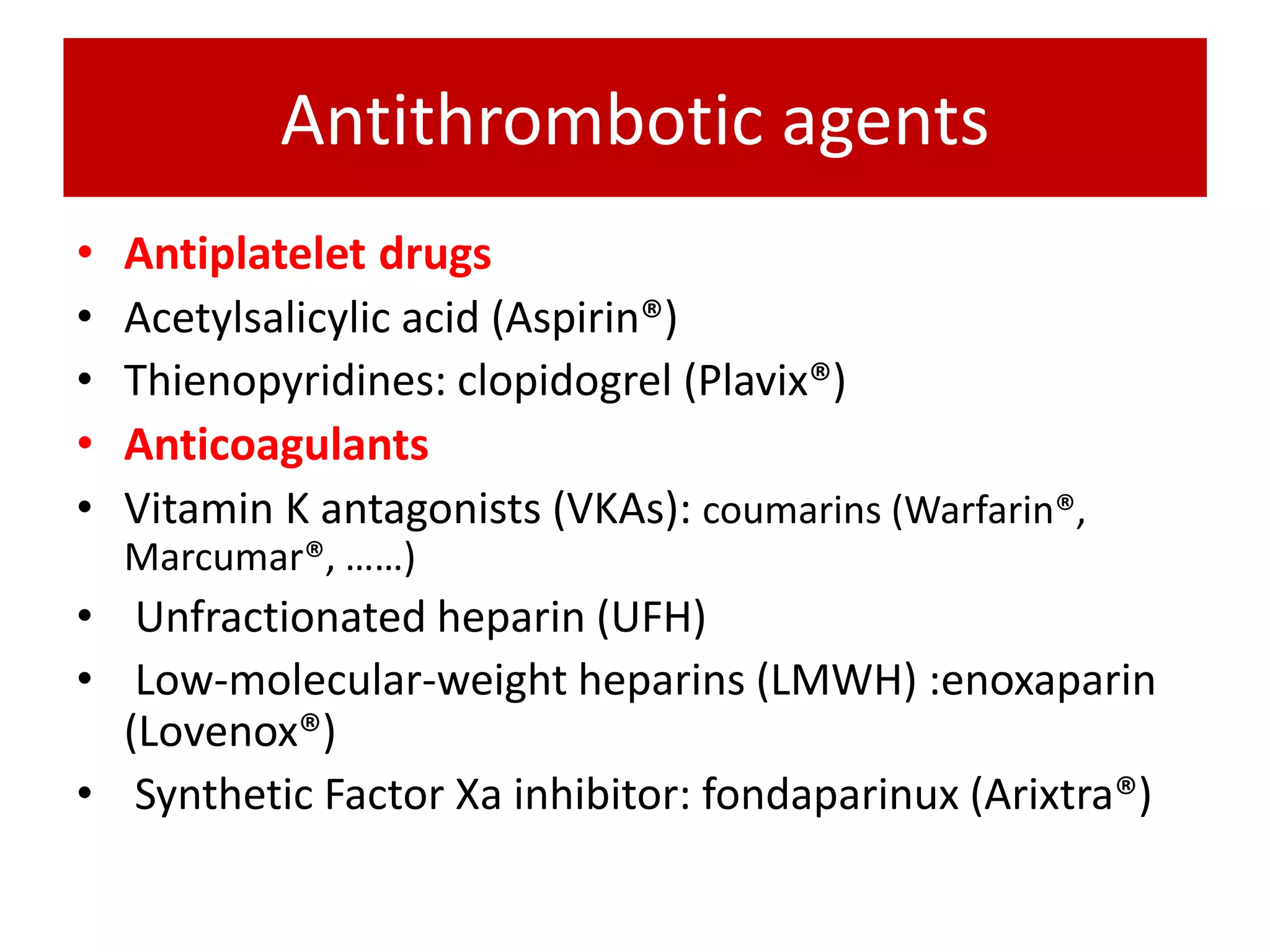
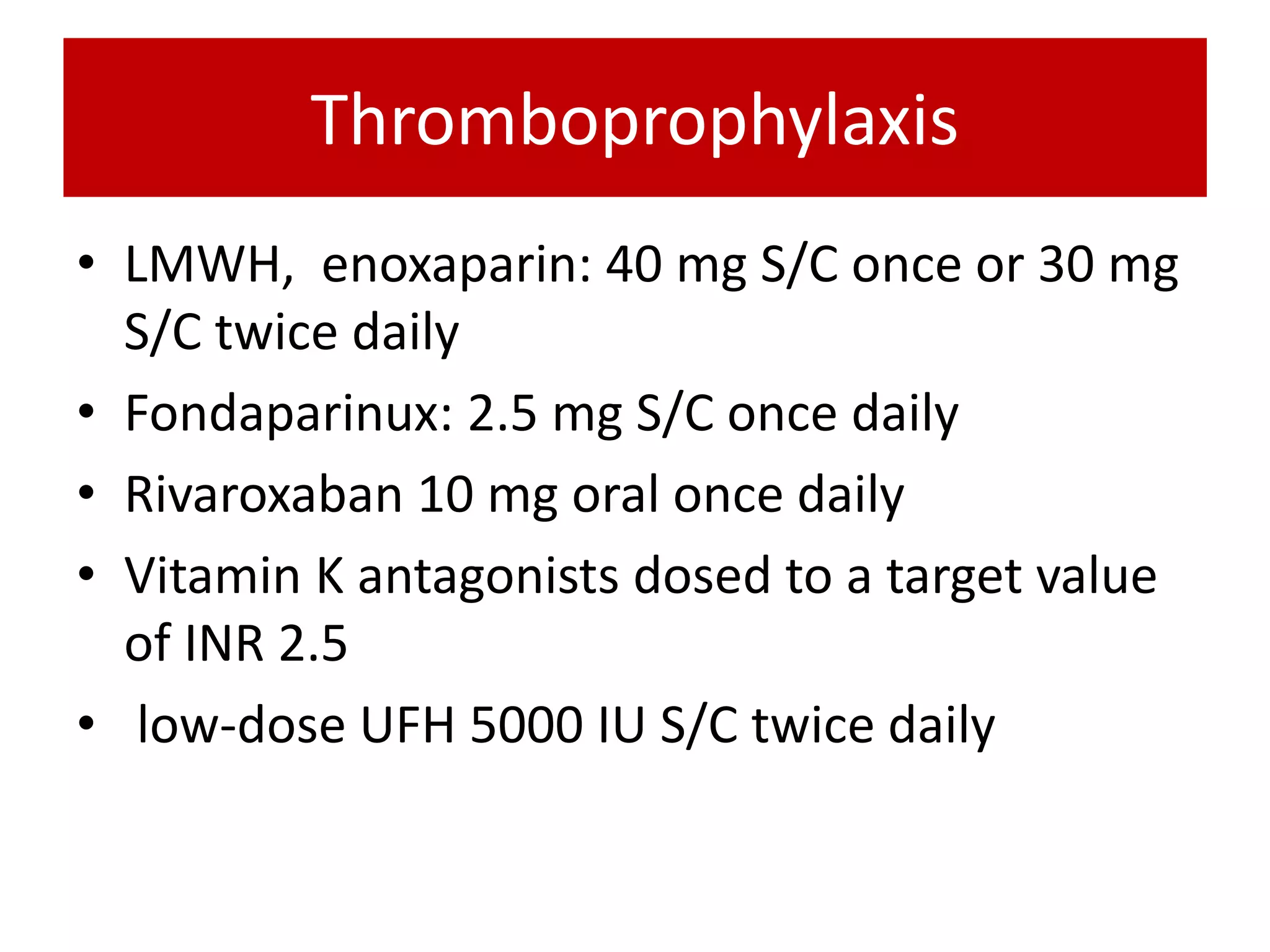
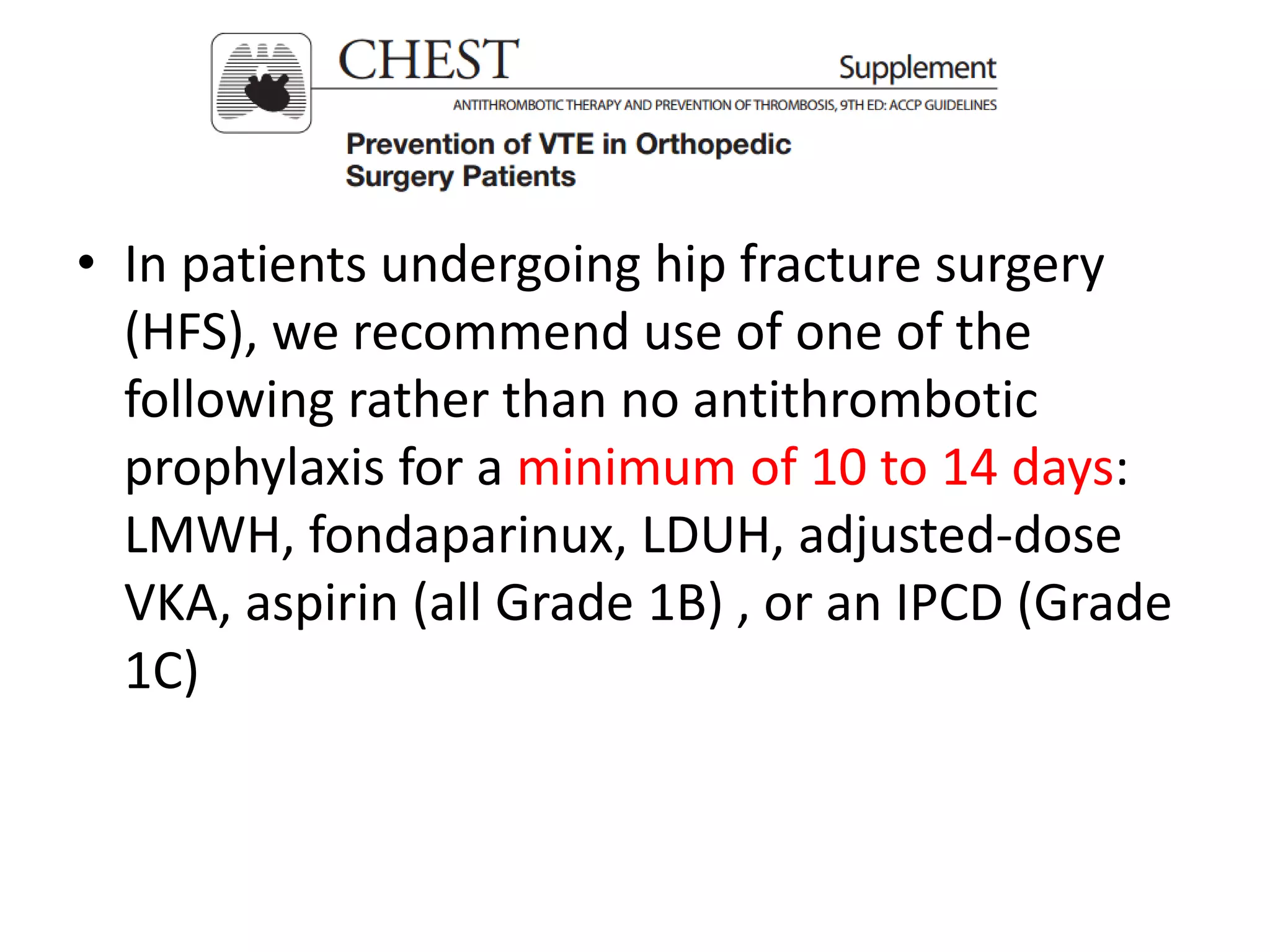
3) Postoperative guidelines recommend thromboprophylaxis including low molecular weight heparin, physical and occupational therapy, and treatment of osteoporosis to improve outcomes for hip fracture patients.