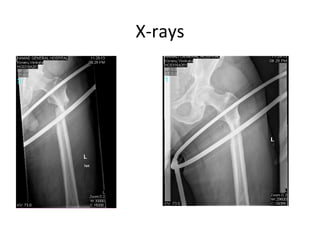
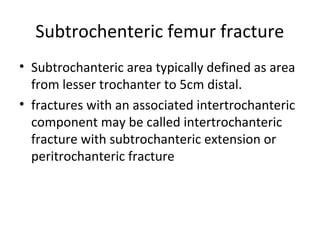
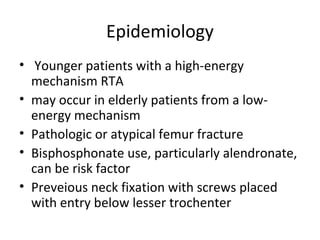
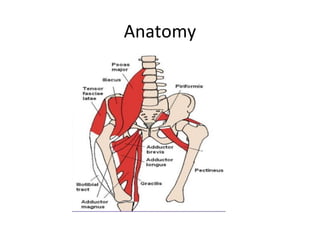
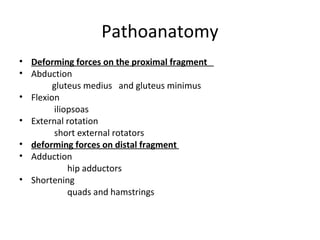
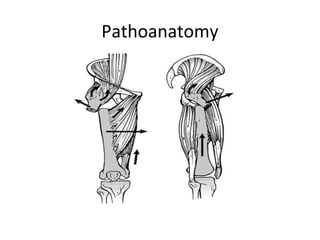
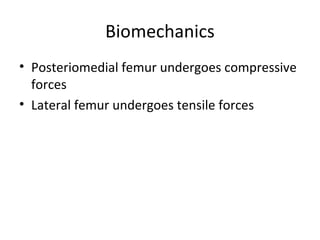
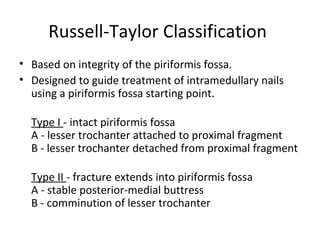
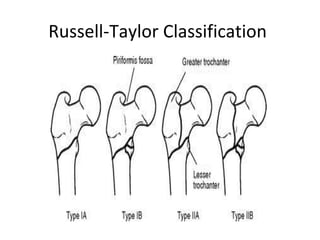
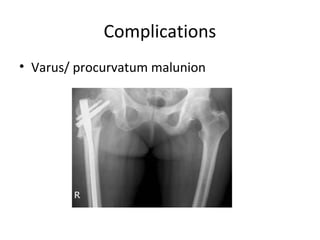
This document summarizes a presentation on subtrochanteric femur fractures. It describes an 80-year-old male patient who presented with hip pain after a fall and was found to have a subtrochanteric femur fracture on x-rays. It then discusses the epidemiology, anatomy, classification, treatment options and complications of subtrochanteric femur fractures, noting that they are most commonly treated with intramedullary nailing. Complications discussed include malunion, nonunion, fixation failure and implant failure.