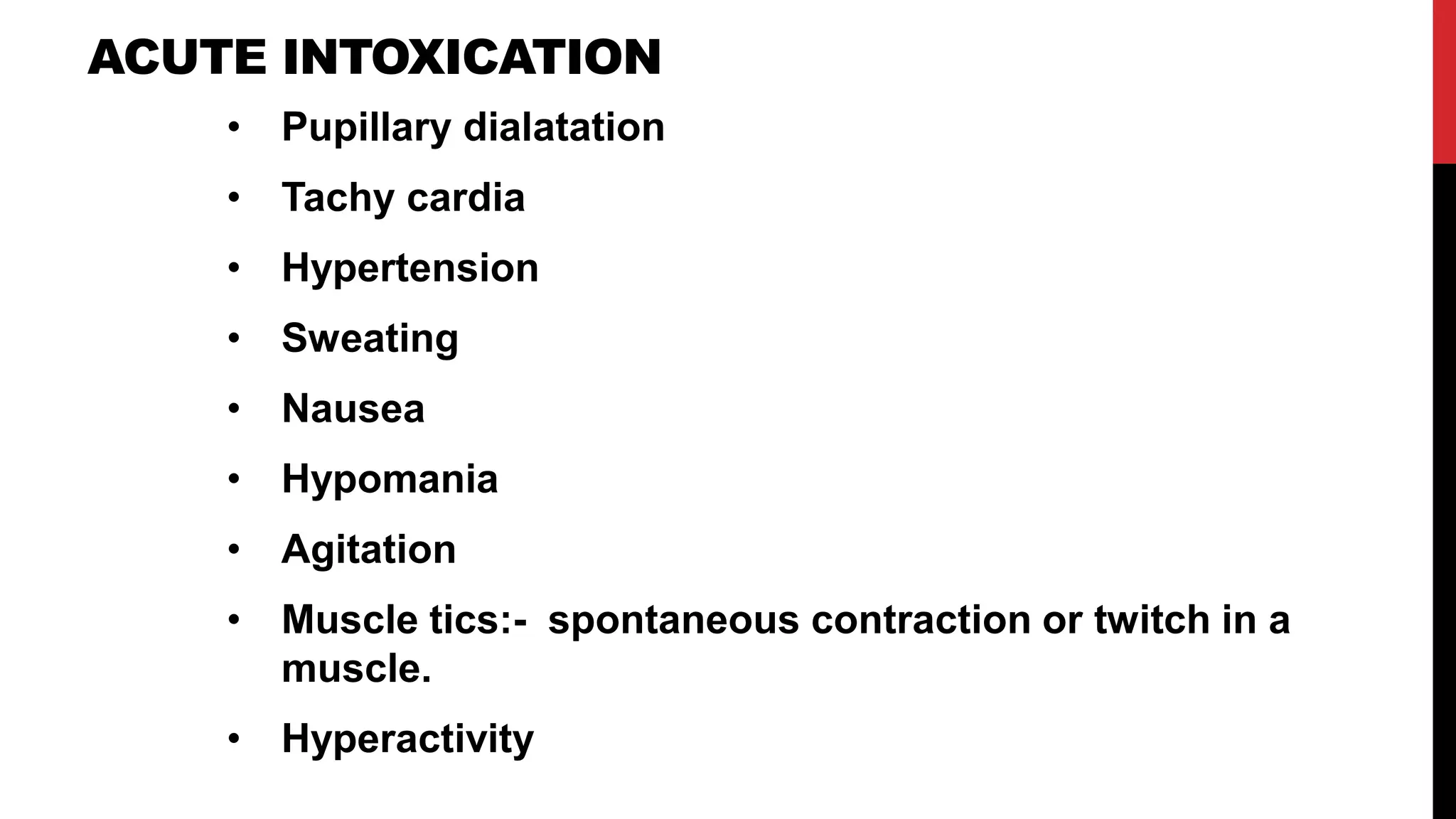
The document discusses substance-related disorders, including definitions and classifications of various substances, the differences between substance abuse, dependence, and intoxication, and the psychological and physical impacts of alcohol. It details diagnostic criteria for alcohol use disorders, phases of alcohol drinking, associated complications, and treatment options such as disulfiram and cognitive therapy. Furthermore, it highlights the epidemiology of alcohol dependence and factors contributing to increased risk, including biological, psychological, and socio-cultural influences.