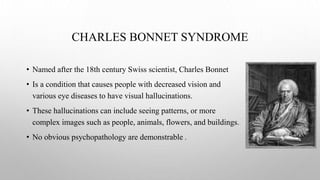
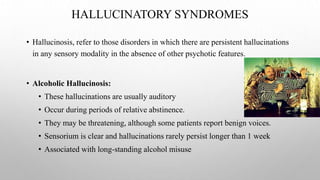
1) The document discusses hallucinations from a psychiatric perspective, covering their history, definitions, causes, and different types.
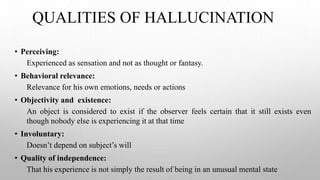
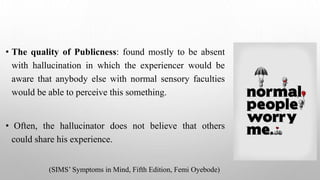
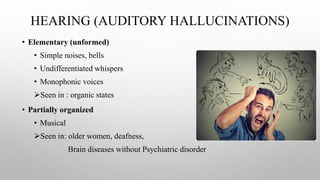
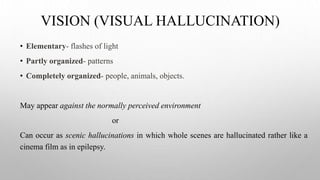
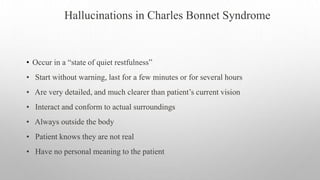
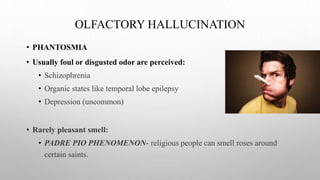
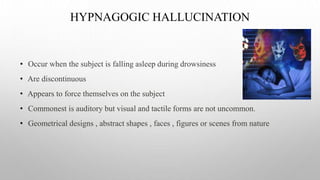
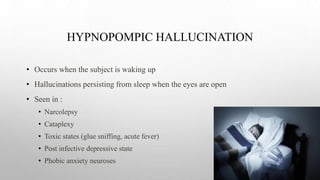
2) Hallucinations are defined as false perceptions that feel real to the patient but are not actually based on an external stimulus. They can affect any of the senses.
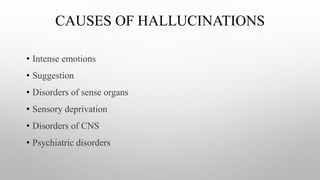
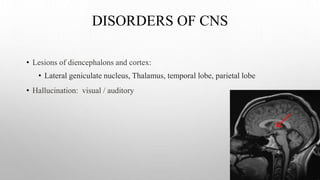
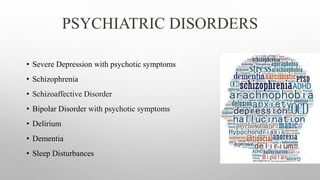
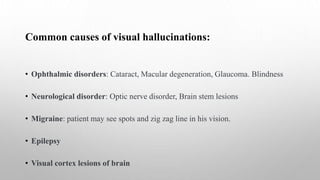
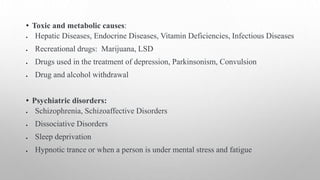
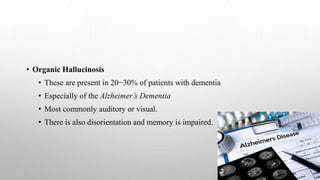
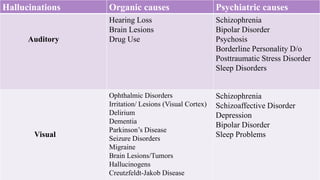
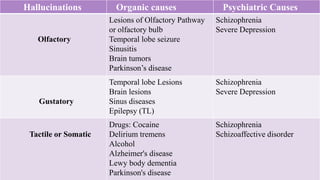
3) Common causes of hallucinations include psychiatric disorders like schizophrenia, substances use, sensory deprivation, neurological disorders, and medical conditions.