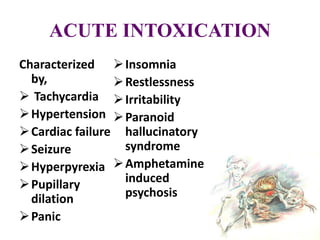
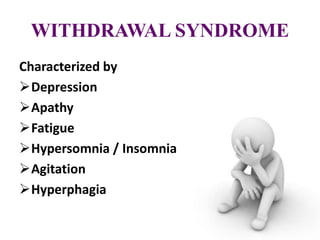
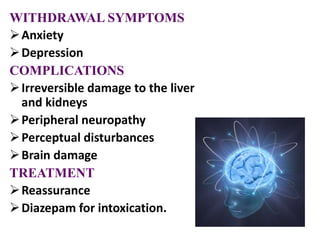
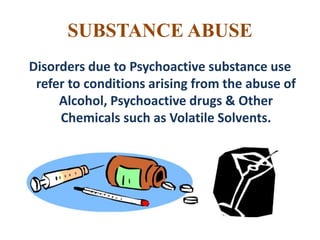
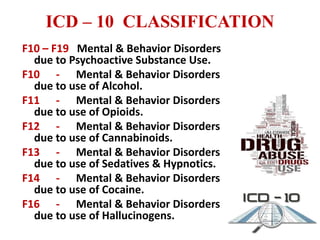
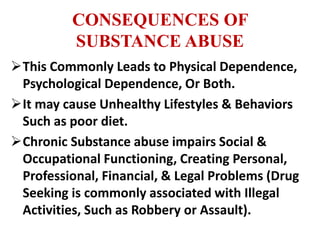
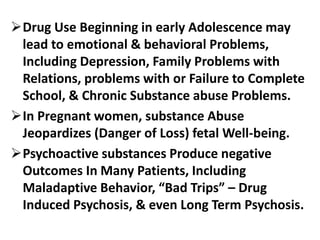
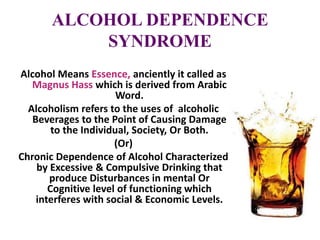
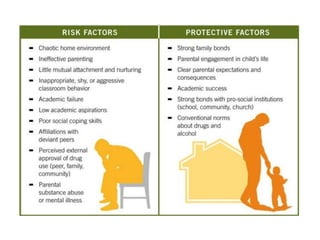
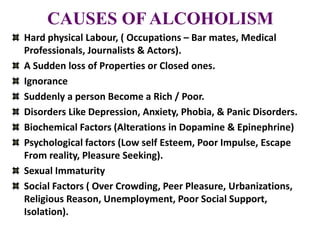
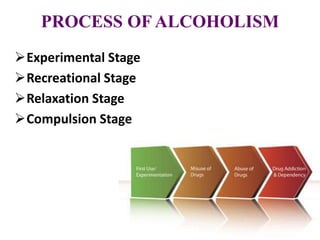
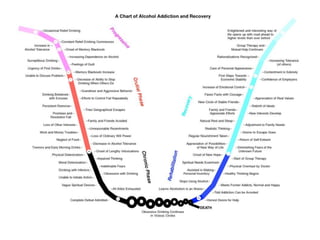
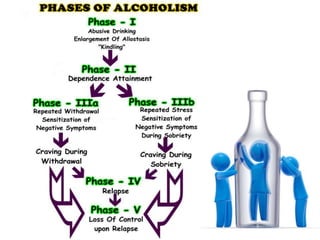
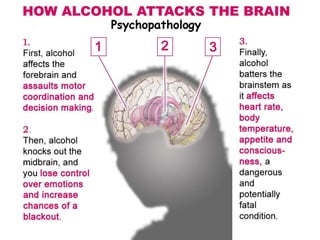
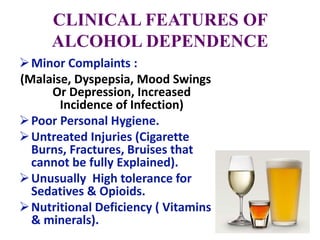
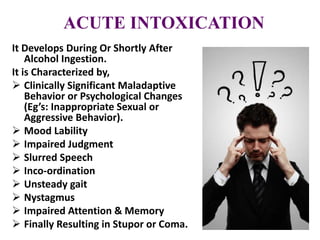
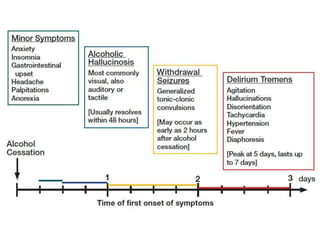
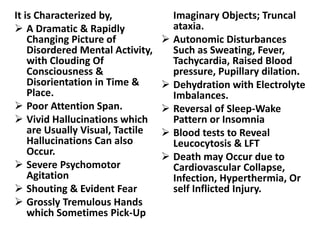
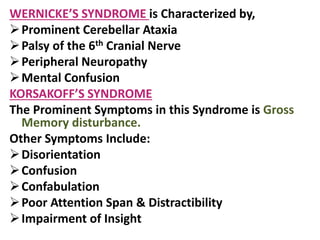
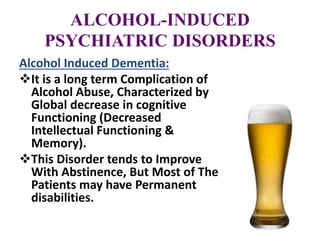
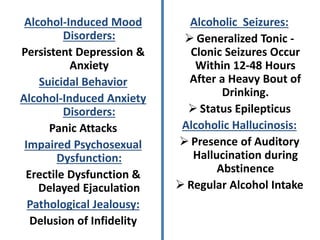
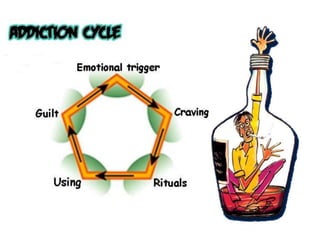
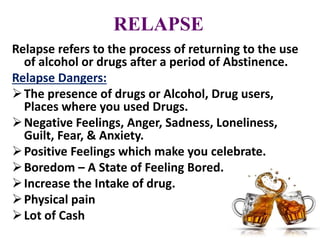
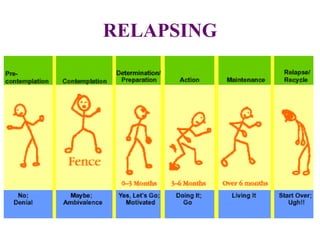
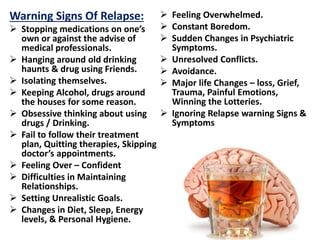
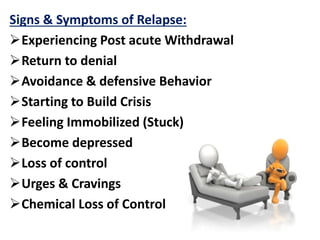
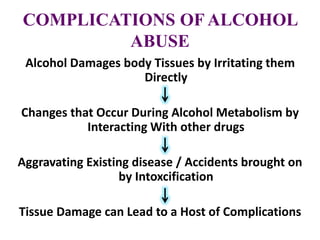
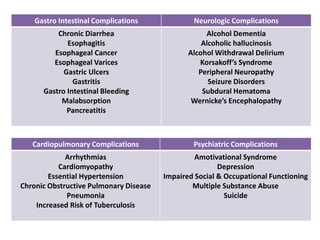
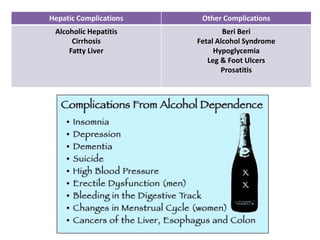
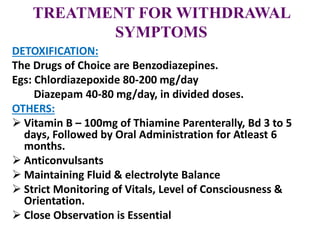
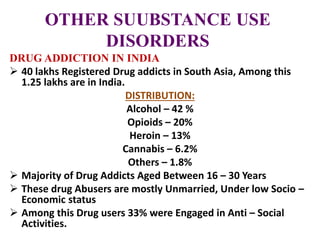
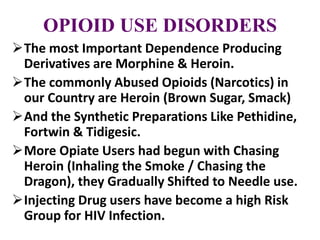
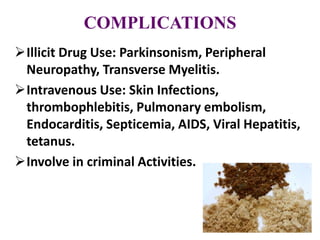
The document discusses substance abuse and alcohol dependence. It defines key terms like substance abuse, addiction, dependence, and withdrawal. It covers the ICD-10 classification of substance use disorders and commonly abused substances. It discusses the etiology of substance abuse from biological, behavioral, psychological, and social perspectives. It provides details on the stages of alcoholism, clinical features of alcohol dependence, and psychiatric disorders caused by alcohol like acute intoxication, withdrawal syndrome, amnestic disorders, and mood disorders. It also covers relapse in alcohol dependence and complications of long-term alcohol abuse.



















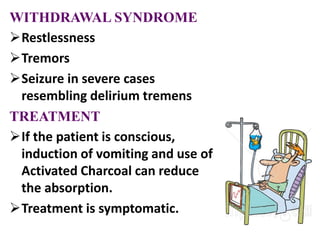
![TREATMENT
Opioid Overdose: Treated with Narcotic Antagonists
[Egs: Naloxone, Naltrexone]
Detoxification: Withdrawal symptoms can be
managed By Methadone, Clonidine, Naltrexone,
Buprenorphine, etc.
Maintenance Therapy: After the Detoxification
Phase, the patient is maintained on one of the
following Regimens:
- Methadone Maintenance
- Opioids Antagonists
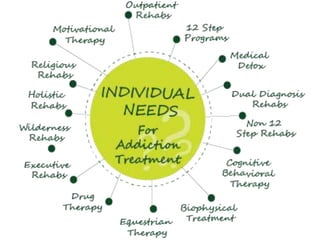
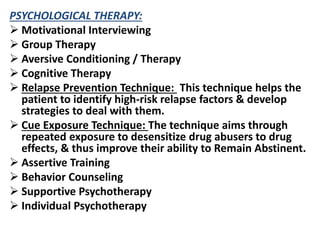
- Psychological methods like Individual
Psychotherapy, Behavior Therapy, Group Therapy,
Family Therapy.](https://image.slidesharecdn.com/substanceabuse-140729014526-phpapp01/85/Substance-Abuse-Psychiatric-Nursing-B-Sc-N-PPT-101-320.jpg)