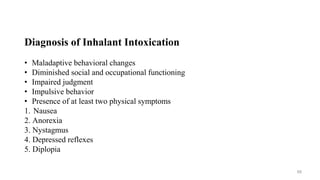
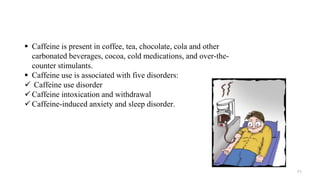
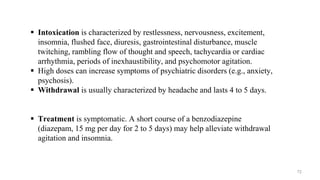
This document provides information on various substance-related disorders, including:
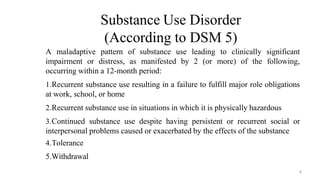
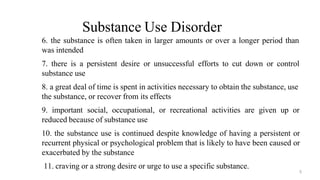
1. It defines substance use disorder according to DSM-5 criteria and lists 11 criteria for diagnosis.
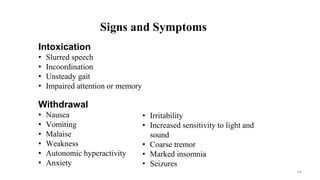
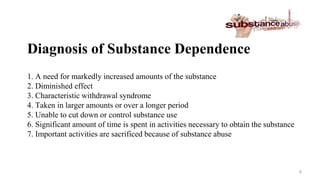
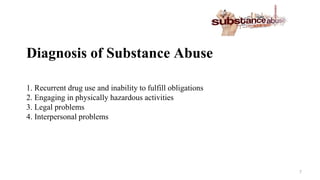
2. It covers terminology related to substance use disorders and describes concepts like dependence, tolerance, withdrawal, and intoxication.
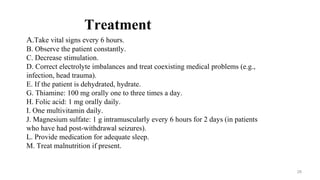
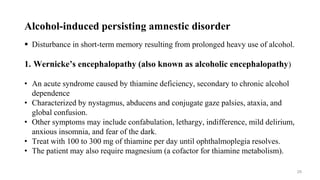
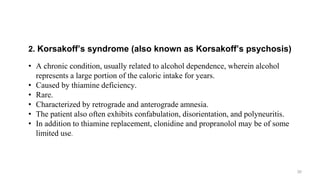
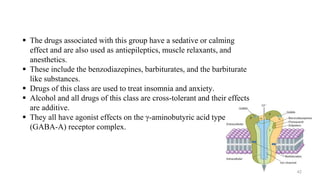
3. It provides details on specific substance use disorders including alcohol, opioids, sedatives, and others. For each it discusses diagnosis, treatment, neurobiology, and more.

![Alcohol withdrawal delirium (delirium tremens [DTs])
Usually occurs only after recent cessation of or reduction in severe, heavy
alcohol use in medically compromised patients with a long history of
dependence
Diagnosis, signs, and symptoms
a. Delirium
b. Marked autonomic
c. Associated features
d. Typical features
27](https://image.slidesharecdn.com/substancerelateddisorders-230801015137-3fc39085/85/substance-related-disorders-pptx-27-320.jpg)