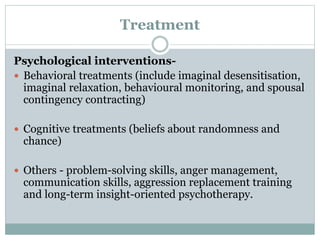
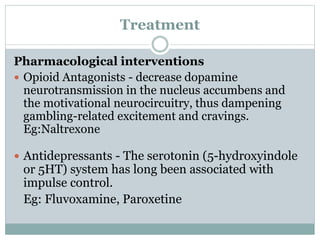
The document reviews various impulse control disorders, including pathological gambling, pyromania, kleptomania, and trichotillomania, discussing their core characteristics, risk factors, prevalence, etiology, and treatments. It emphasizes the psychological and pharmacological interventions available for these disorders, alongside the high comorbidity with substance use and mood disorders. Additionally, a study on impulse control disorders in Parkinson's disease patients highlights significant findings regarding their prevalence and associated factors.

![(F63) HABIT AND IMPULSE DISORDERS
F63.0 PATHOLOGICAL GAMBLING
F63.1 PATHOLOGICAL FIRE-SETTING
[PYROMANIA]
F63.2 PATHOLOGICAL STEALING
[KLEPTOMANIA]
F63.3 TRICHOTILLOMANIA
F63.8 OTHER HABIT AND IMPULSE
DISORDERS
F63.9 HABIT AND IMPULSE DISORDER,
UNSPECIFIED](https://image.slidesharecdn.com/impulsecontroldisorder-161009113348/85/Impulse-control-disorder-4-320.jpg)



![F63.1 PATHOLOGICAL FIRE-SETTING
[PYROMANIA]
The disorder is characterized by multiple acts of, or
attempts at, setting fire to property or other objects,
without apparent motive, and by a persistent
preoccupation with subjects related to fire and burning.
There may also be an abnormal interest in fire-engines
and other fire-fighting equipment, in other associations
of fires, and in calling out the fire service.
The population prevalence of pyromania is not known.](https://image.slidesharecdn.com/impulsecontroldisorder-161009113348/85/Impulse-control-disorder-10-320.jpg)



![F63.2 PATHOLOGICAL STEALING
[KLEPTOMANIA]
The disorder is characterized by repeated failure to
resist impulses to steal objects that are not acquired
for personal use or monetary gain.
The Objects may instead be discarded, given away, or
hoarded. The disorder may cause legal, family,
career, and personal difficulties.](https://image.slidesharecdn.com/impulsecontroldisorder-161009113348/85/Impulse-control-disorder-14-320.jpg)









