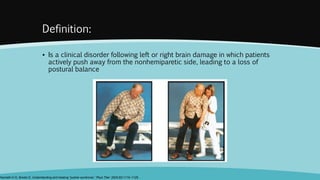
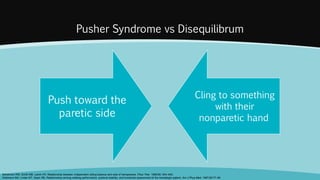
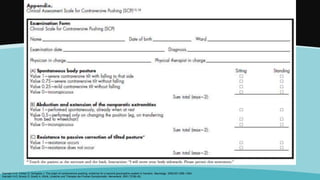
Pusher syndrome is a disorder following brain damage where patients actively push away from their non-paretic side, losing postural balance. It is caused by damage to the posterolateral thalamus, altering perception of the body's orientation to gravity. Treatment focuses on helping patients visually explore their surroundings to recognize their tilted posture. Prognosis is generally good, with function often recovering within 6 months.