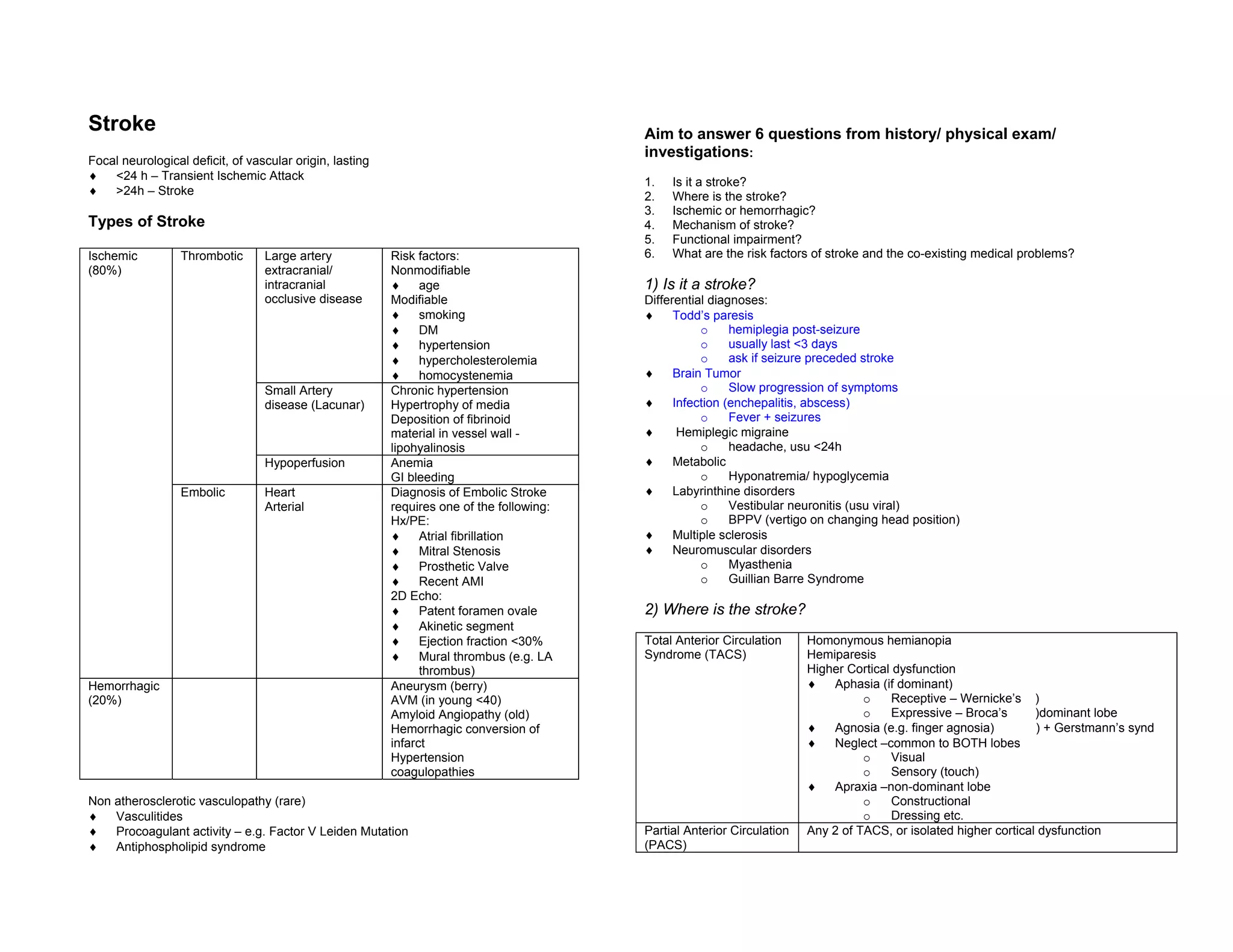
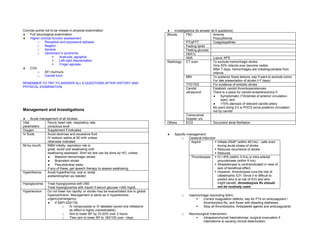
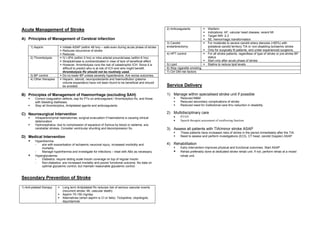
The document provides guidance on evaluating and managing patients presenting with suspected stroke. It outlines an approach to answering 6 key questions from the history, physical exam, and investigations to determine if the patient is having a stroke, identify the location and type of stroke, understand the mechanism, assess functional impairment, and identify risk factors. Principles of acute management include aspirin, thrombolysis if eligible, controlling blood pressure and blood glucose, and preventing hyperthermia. Secondary prevention involves antiplatelet therapy, anticoagulation if indicated, carotid endarterectomy for severe stenosis, controlling hypertension and lipids, smoking cessation, and managing diabetes risk factors.