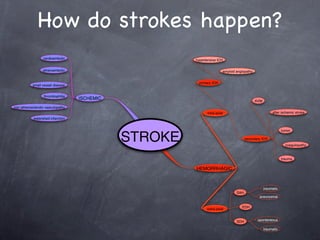
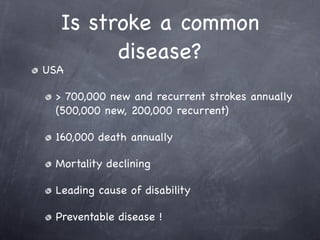
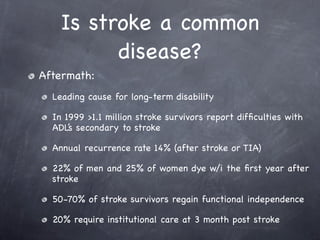
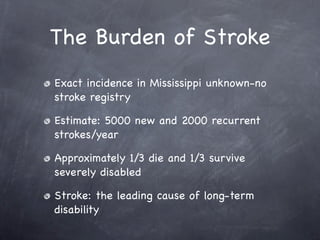
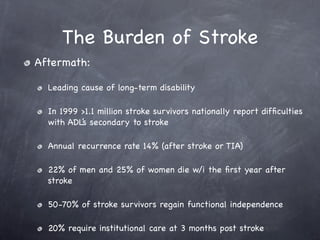
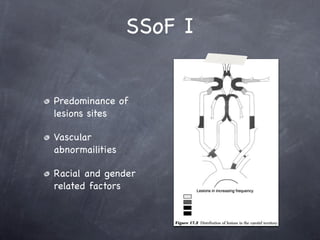
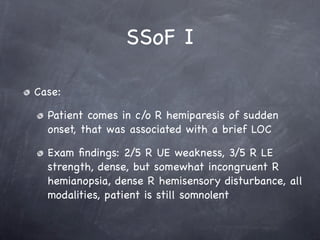
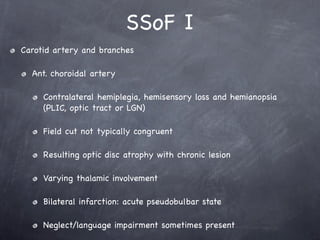
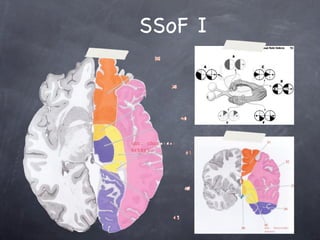
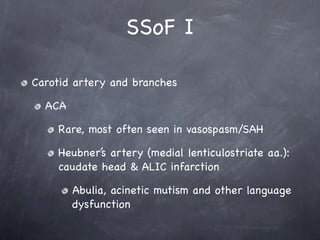
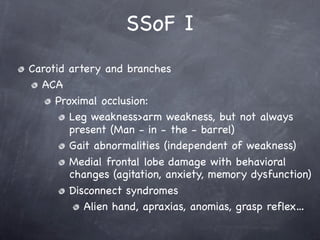
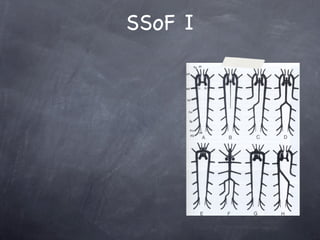
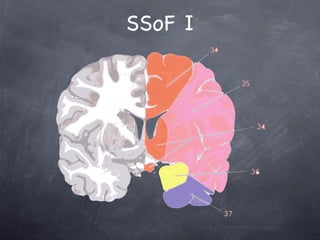
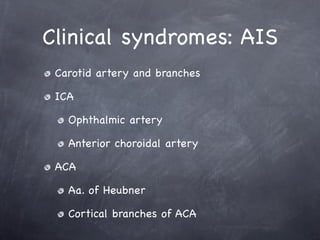
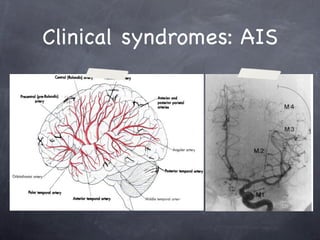
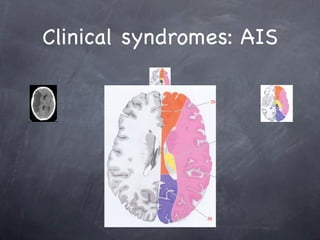
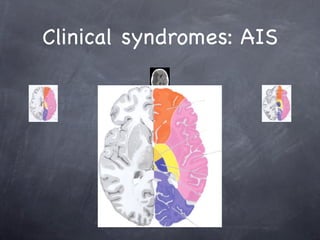
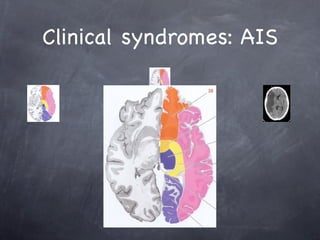
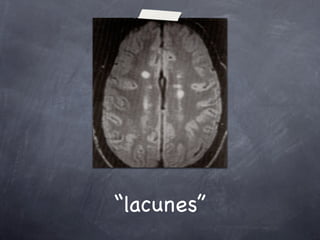
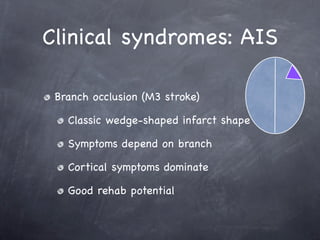
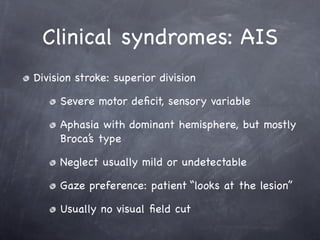
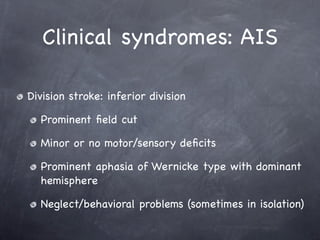
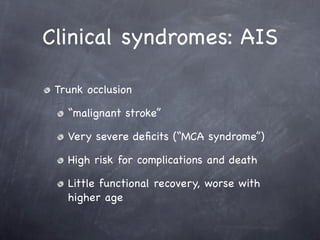
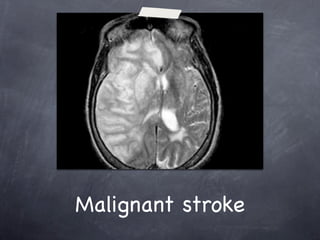
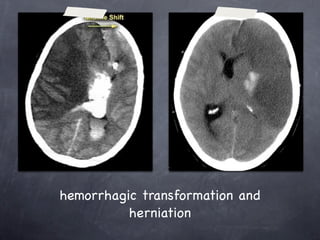
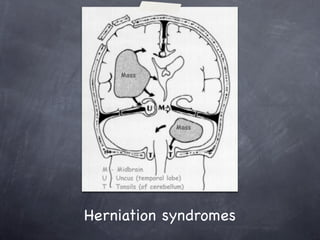
This document discusses stroke syndromes of the forebrain. It begins by defining what a stroke is and describing the most common causes. It then discusses how strokes occur based on the specific blood vessels affected, such as the carotid artery and its branches. It notes that stroke is a very common condition in the US, with over 700,000 new and recurrent strokes annually. The rest of the document goes into more detail about specific stroke syndromes based on the location of blockages or ruptures in the arteries supplying the brain. It describes syndromes associated with different branches and divisions of the middle cerebral artery. Larger blockages cause more severe deficits and higher risks of complications.