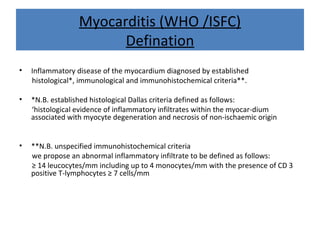
1. Myocarditis is an inflammatory disease of the myocardium diagnosed using histological, immunological and immunohistochemical criteria, with an abnormal inflammatory infiltrate defined as ≥14 leucocytes/mm including up to 4 monocytes/mm and ≥7 CD3 positive T-lymphocytes/mm.
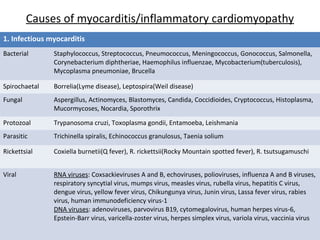
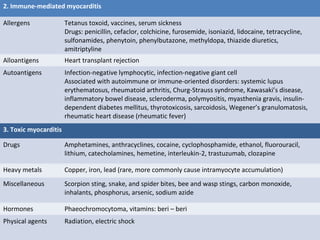
2. Causes of myocarditis include infectious agents like viruses, bacteria, and parasites; immune-mediated reactions to drugs, vaccines or transplants; and toxic effects of drugs, heavy metals, and other toxins.
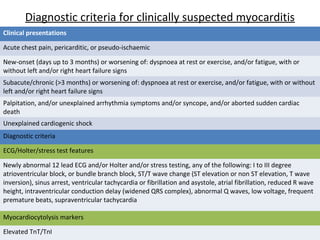
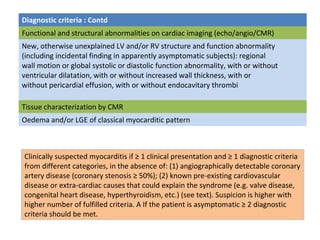
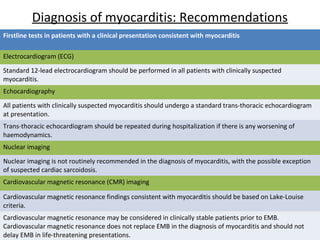
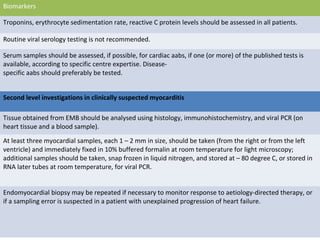
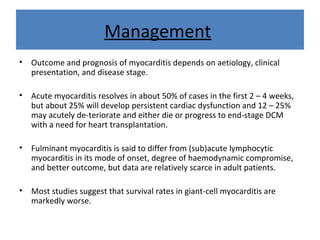
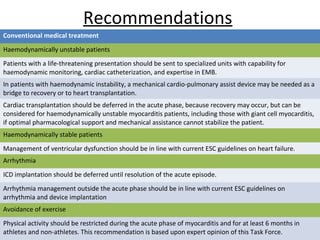
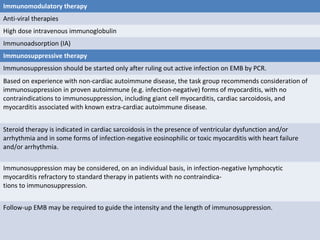
3. Diagnosis involves clinical presentations like chest pain and heart failure, as well as diagnostic criteria including ECG/imaging abnormalities, elevated cardiac biomarkers, and endomyocardial biopsy showing