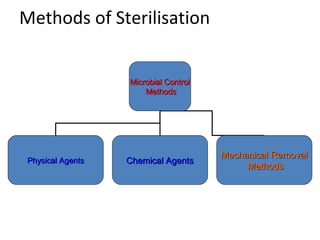
This document discusses sterilization and disinfection methods. It defines sterilization as the process of removing all microorganisms, including spores, while disinfection reduces microorganisms to non-disease causing levels. Physical sterilization methods include heat (dry heat, moist heat like autoclaving), radiation, and filtration. Chemical methods use substances like alcohols, aldehydes, halogens, dyes, phenols, and biguanides. Proper sterilization requires management systems, facilities, equipment, trained staff, and record keeping to be effective.