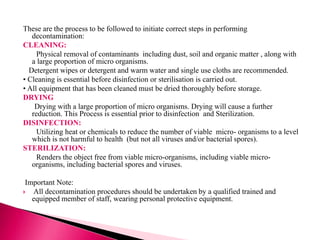
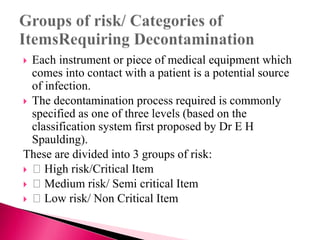
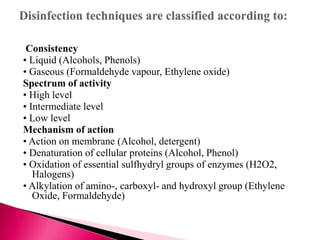
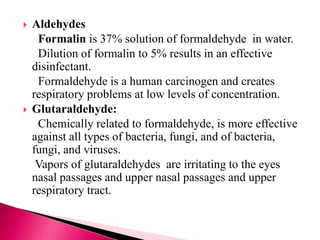
The document discusses various methods and processes for decontaminating medical equipment. It defines key terms like contamination, decontamination, cleaning, drying, disinfection and sterilization. It describes the three levels of risk for medical equipment based on its contact with patients - high, medium and low risk. For each level, it recommends the appropriate decontamination process - sterilization for high risk equipment, sterilization or disinfection for medium risk, and cleaning for low risk. It then discusses the various processes in detail, including manual and automated cleaning methods, types of disinfectants and disinfection methods, and sterilization techniques like heat, radiation and filtration.
![TOPIC :BARRIER NURSING[Decontamination of
equipments and unit ]
Prepared By:Mrs BeminaJA
Assistant Professor
ESIC College of Nursing
Kalaburagi](https://image.slidesharecdn.com/decontamination-220923052835-a5eb5248/85/DECONTAMINATION-pptx-1-320.jpg)