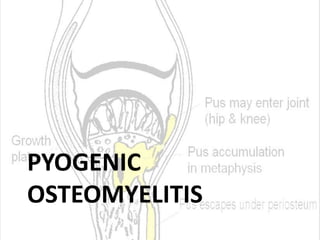
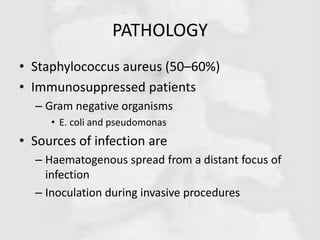
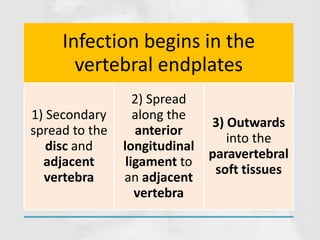
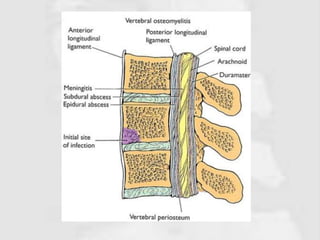
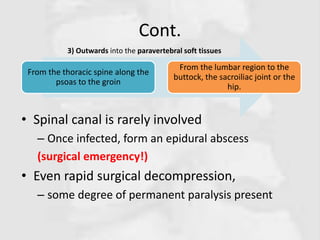
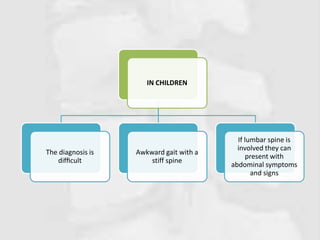
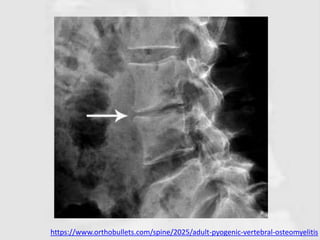
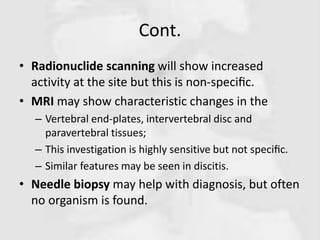
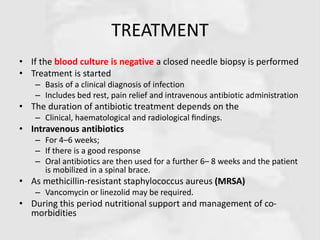
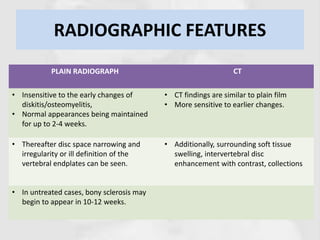
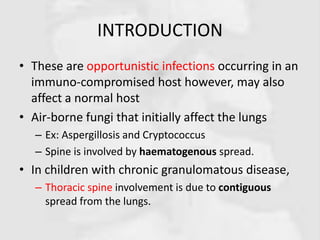
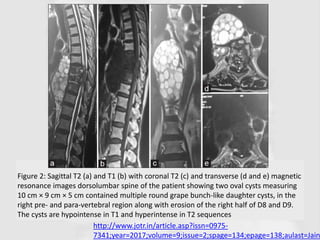
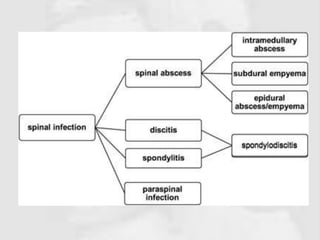
The document discusses various types of spine infections including pyogenic osteomyelitis, discitis, fungal spine infections, and parasitic infections. It covers the definition, etiology, risk factors, clinical features, investigations, and management for each type. Key points include that pyogenic osteomyelitis most commonly affects the elderly or immunocompromised, discitis usually results from invasive procedures, fungal infections occur in immunocompromised patients, and echinococcus granulosus is a common parasitic infection in sheep-raising areas. Treatment involves antibiotics, surgery if needed, and addressing any underlying risks.