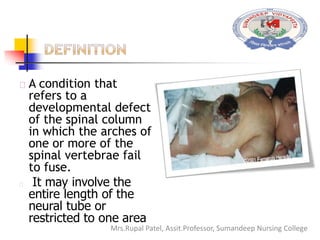
Spinal bifida is a birth defect where the spinal column does not fully close around the spinal cord. It can range from mild where there are no symptoms to severe where nerves and the cord itself protrude out of the open spine. Causes include genetic factors and folic acid deficiency. Treatment depends on severity but may include surgery to close the opening and address any complications like hydrocephalus. Nursing care focuses on preventing infection, monitoring for complications, and teaching parents how to care for the child's needs.