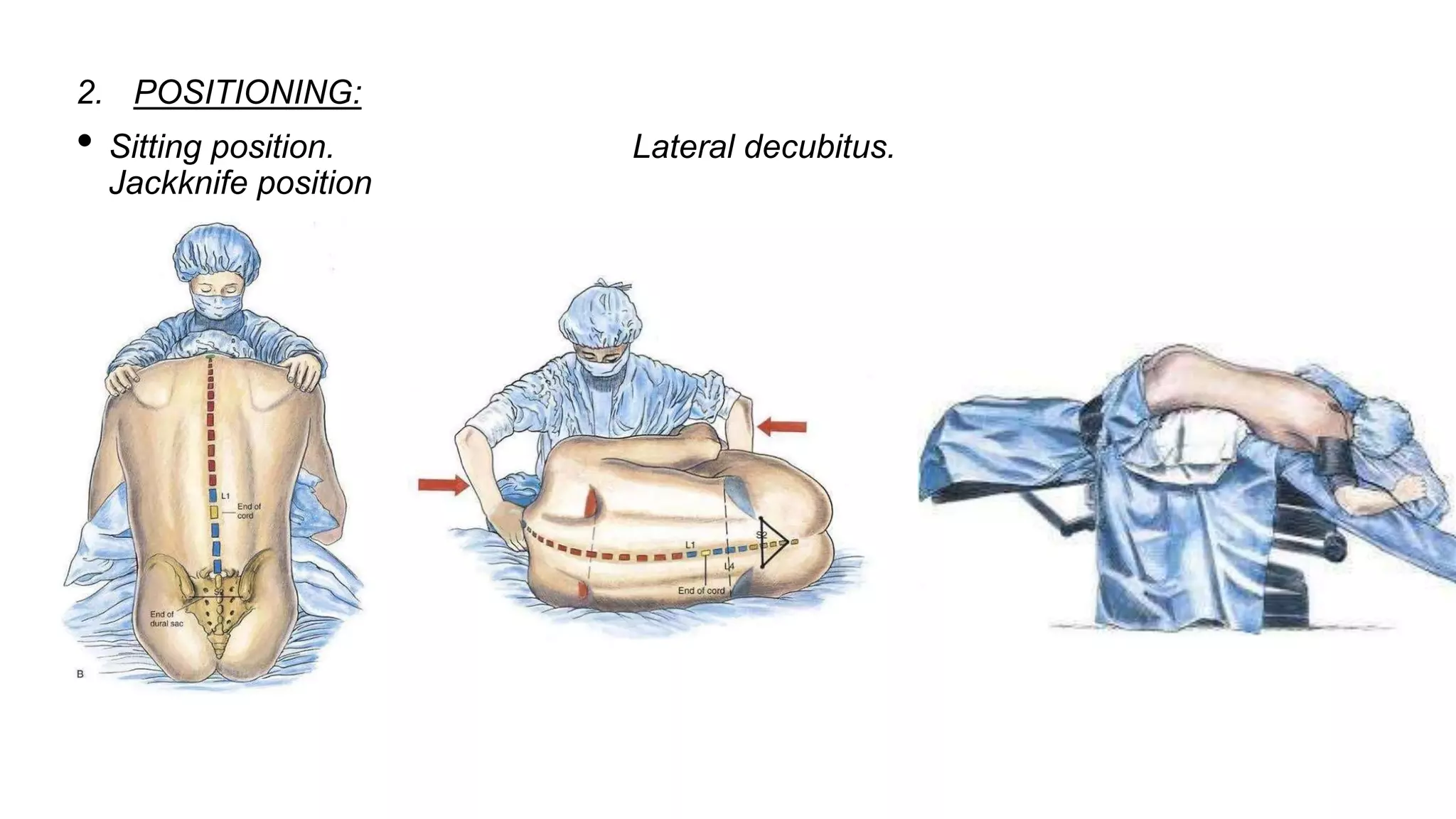
Spinal anaesthesia involves injecting local anaesthetic into the subarachnoid space to block nerve impulses from the lower half of the body. It was first performed in 1898 and involves accessing the spinal canal between vertebrae to administer drugs. Proper patient positioning, needle selection, and drug choice are important to achieve the desired level and duration of anaesthesia while avoiding complications like hypotension, neurological issues, or infection. Close monitoring is needed due to potential effects on heart rate, breathing, and blood pressure.