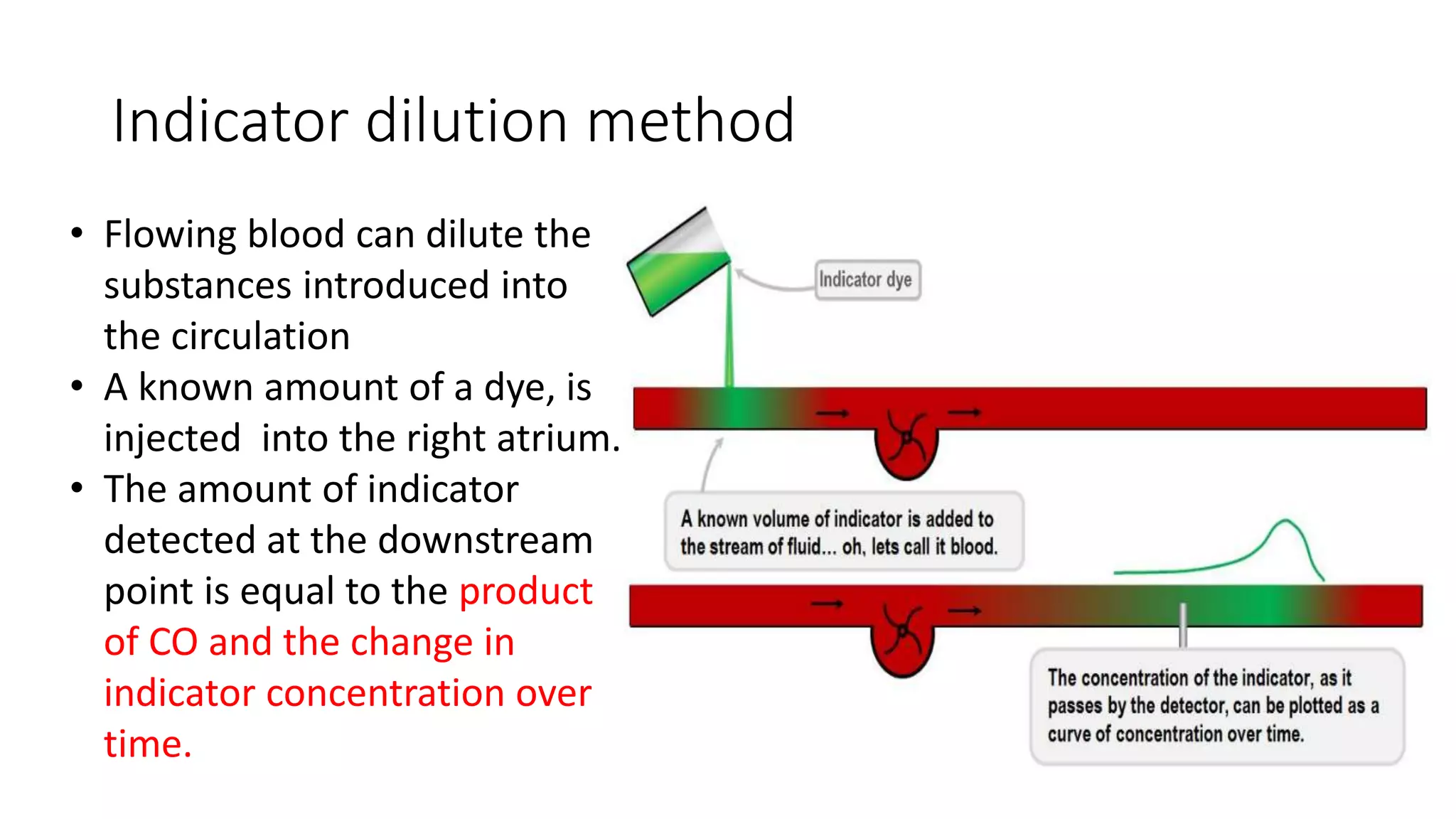
Cardiac output monitoring can be done using invasive, minimally invasive, and non-invasive methods. Invasive methods like pulmonary artery catheter use thermodilution or dye dilution to directly measure cardiac output but carry risks. Minimally invasive methods like LiDCO, PiCCO, and FloTrac use pulse contour analysis after initial calibration. Non-invasive options include thoracic bioimpedance and echocardiography. The choice of monitoring method depends on factors like accuracy, ease of use, risks, and costs. While goal-directed therapy using cardiac output monitoring may improve outcomes in some high-risk patients, large trials found no clear benefit of pulmonary artery catheters on mortality.















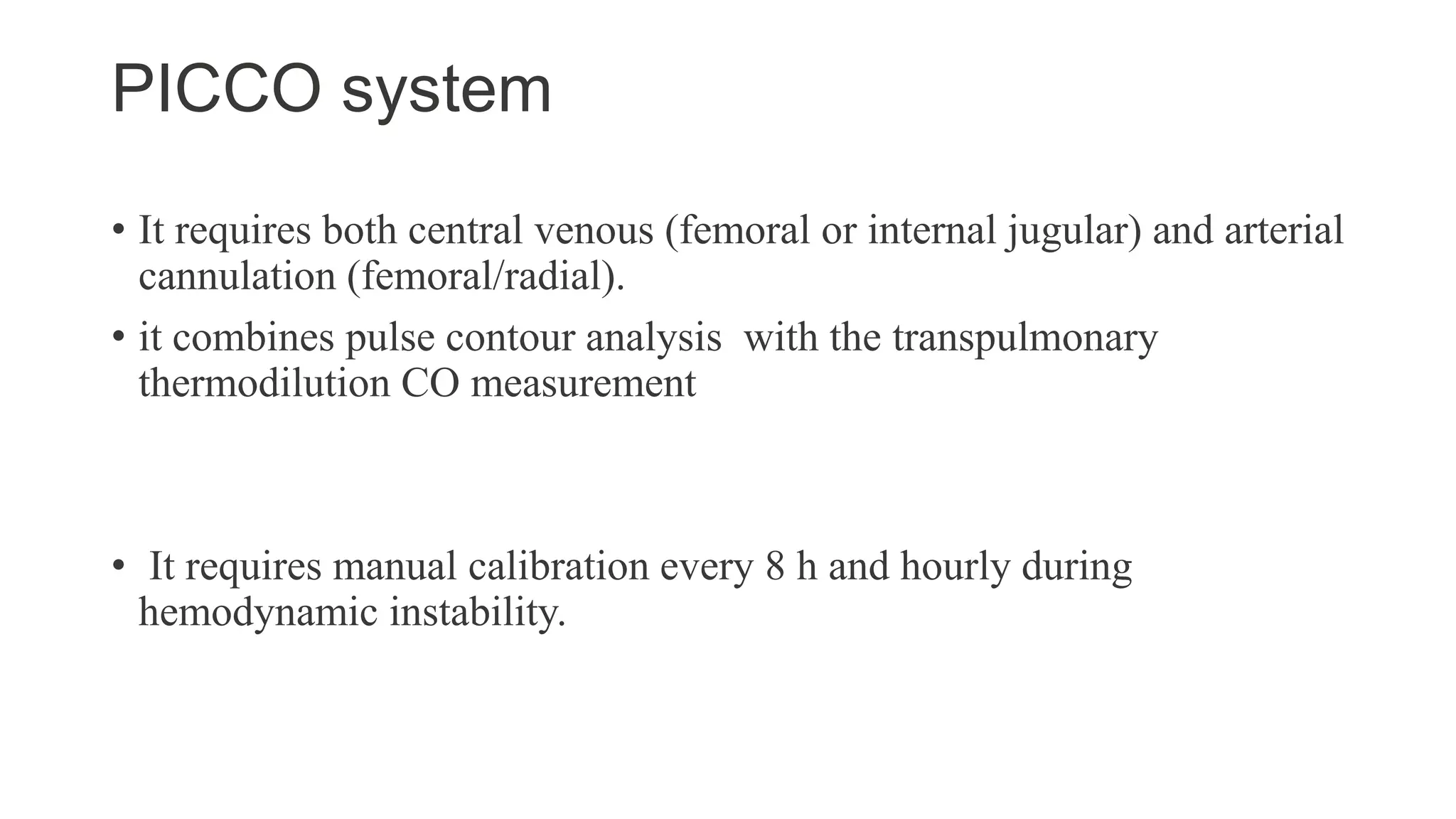
![Pulse Contour Analysis - Principle
t [s]
P [mm Hg]
Area under
pressure curve
Shape of
pressure curve
PCCO = cal • HR •
Systole
P(t)
SVR
+ C(p) •
dP
dt
( ) dt
Aortic
compliance
Heart
rate
Patient-specific calibration factor
(determined by thermodilution)
• Arterial pressure waveform determined by interaction of
stroke volume and SVR.
• based on the principle that area under the systolic part
of the arterial pressure waveform is proportional to the
SV.](https://image.slidesharecdn.com/cardiacoutputautosaved-221227070826-6a681946/75/cardiac-output-pptx-19-2048.jpg)