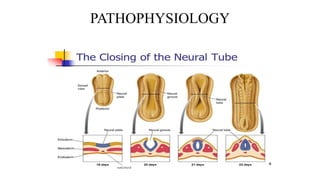
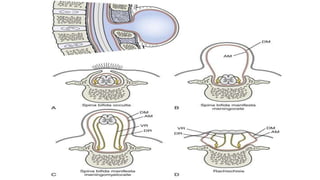
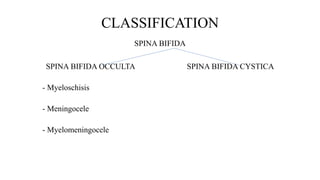
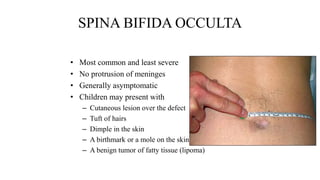
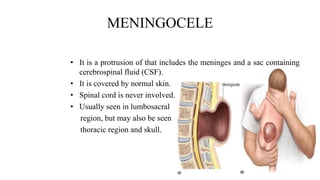
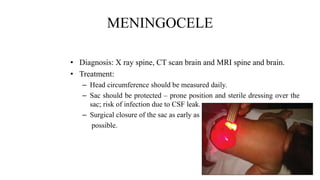
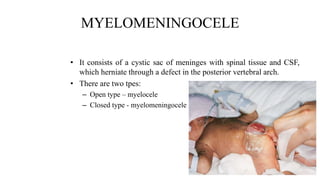
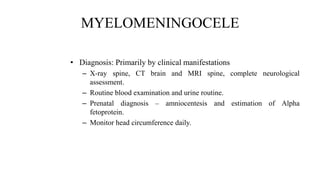
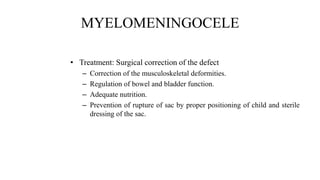
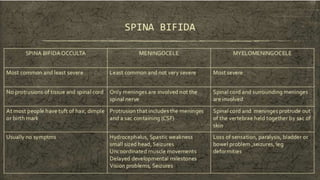
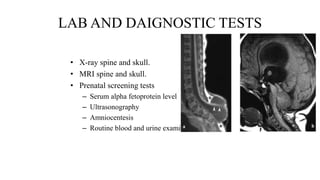
This document provides information about Spina Bifida, a neural tube birth defect where there is incomplete closing of the neural arches and meninges around the spinal cord. It describes the classification and types of Spina Bifida (occulta, meningocele, myelomeningocele), symptoms, diagnosis using imaging and tests, and treatment options which may include surgery to close the opening and manage related issues like hydrocephalus. It emphasizes the importance of emotional support for parents and monitoring the infant's health and development.