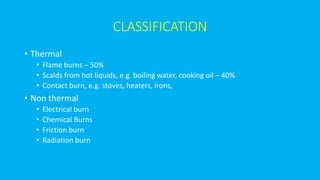
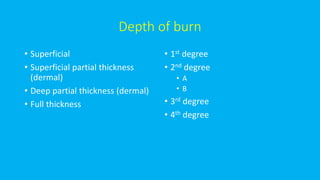
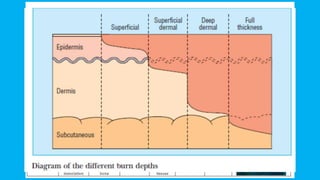
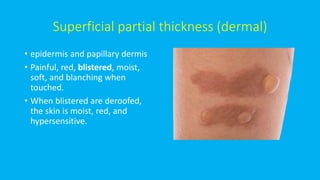
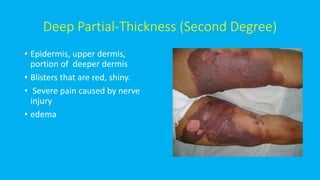
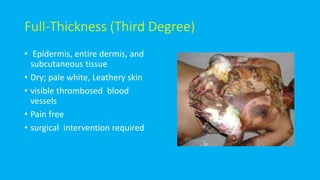
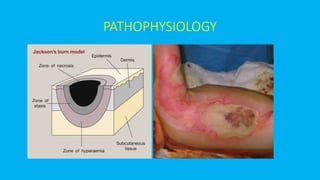
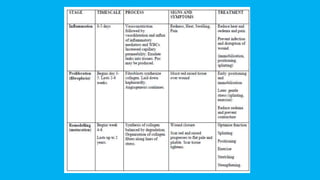
1) Burns are classified based on depth and cause, with thermal burns being the most common. Depth ranges from superficial to full thickness burns.
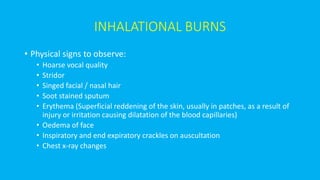
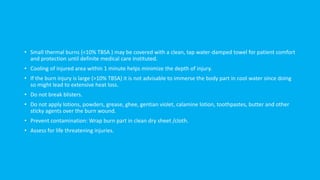
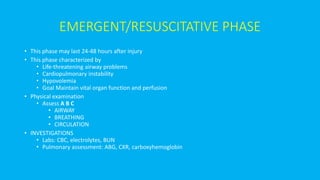
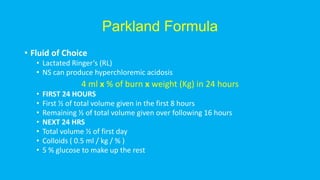
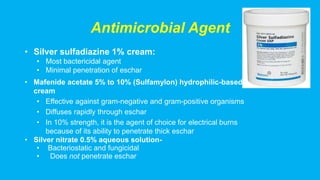
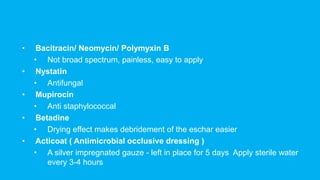
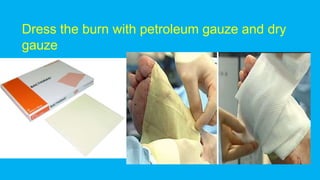
2) Initial management focuses on airway, breathing, circulation, and fluid resuscitation to prevent shock. Wound care aims to prevent infection using antimicrobial dressings.
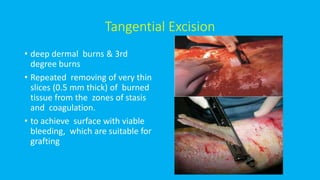
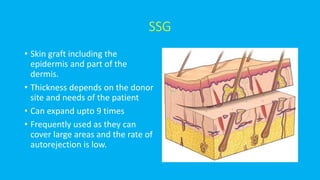
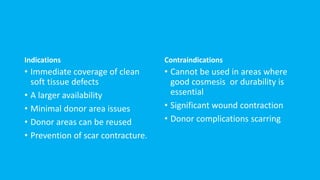
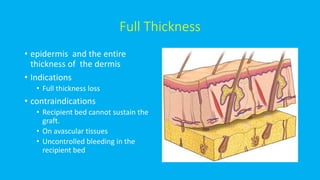
3) Later stages involve wound debridement and skin grafting to promote healing, along with managing pain and nutrition. Early excision within 5 days of injury reduces risk of sepsis.