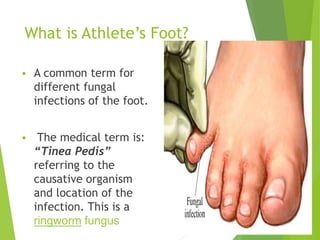
Athlete's foot, also known as tinea pedis, is a common fungal infection of the feet caused by dermatophytes that thrive in warm, moist environments. It is contracted through direct contact with infected skin or surfaces like floors, locker rooms, or footwear. Symptoms include cracked, flaking, peeling skin between the toes or on the foot that is red, itchy, and painful. Diagnosis is usually made by visual examination and may include skin cultures or biopsies. Treatment involves using over-the-counter antifungal creams and powders for 1-2 weeks. Preventive measures include keeping feet dry, changing socks daily, and wearing well-ventilated shoes.










![Treatment
Keep feet clean and dry (especially interdigital [in-
between the feet] )
Thorough feet wash with soap and water
Dry completely and carefully (Twice daily)
Wear clean cotton socks
Change socks as often as necessary to keep feet
dry.
Its responds well to self care, but may recur.
12](https://image.slidesharecdn.com/slidesathletesfootv2-150723182942-lva1-app6891/85/Slides-athletes-footv2-12-320.jpg)





