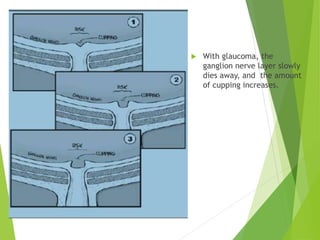
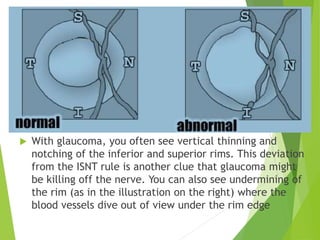
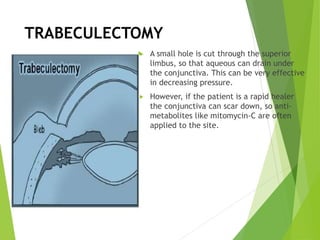
Glaucoma is a disease where the optic nerve dies, leading to irreversible vision loss. There are two main types - open-angle and closed-angle glaucoma. Open-angle glaucoma is more common and occurs when drainage of the aqueous humor is blocked, causing chronic high pressure in the eye. Closed-angle glaucoma is an emergency where the drainage angle suddenly closes, rapidly increasing pressure and damaging vision within hours if not treated. Treatment focuses on lowering pressure through eye drops or surgery.