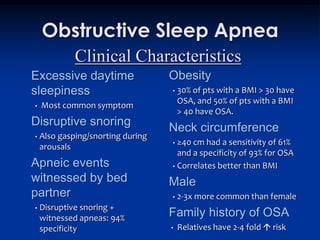
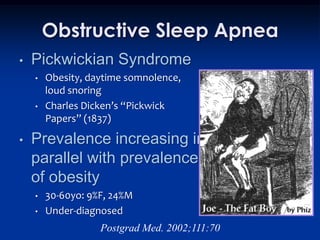
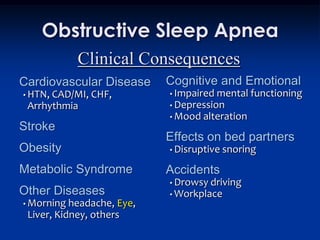
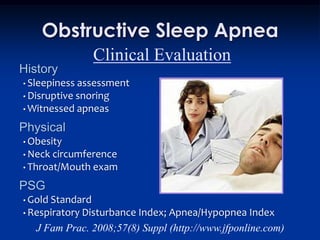
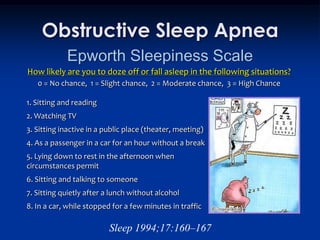
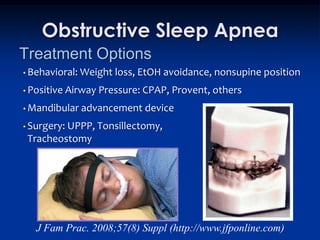
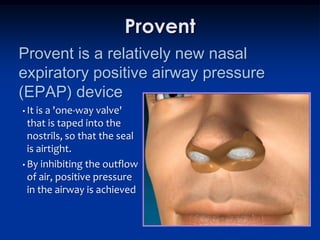
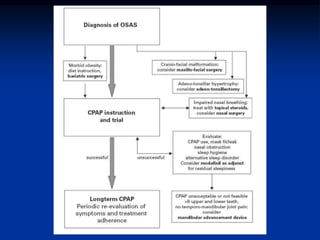
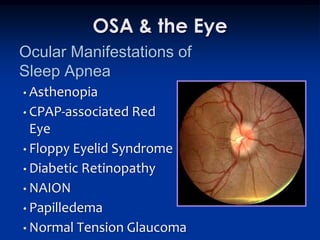
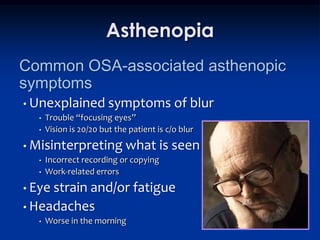
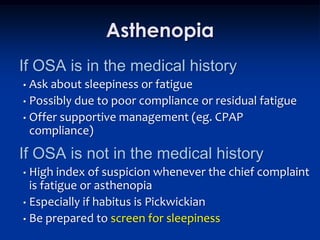
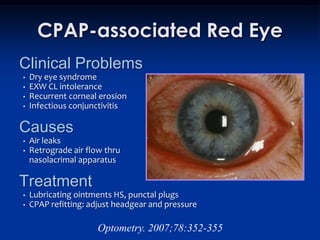
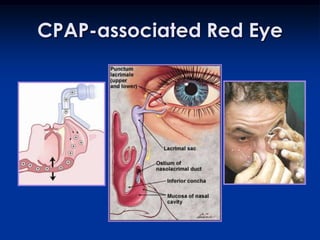
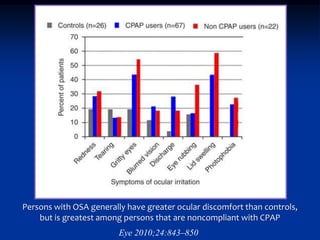
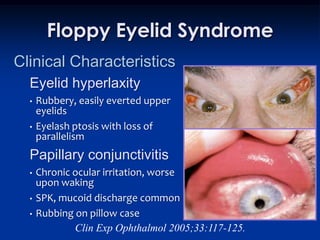
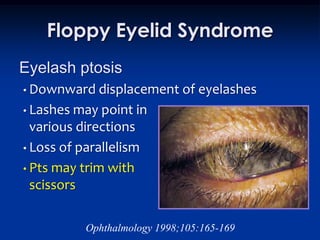
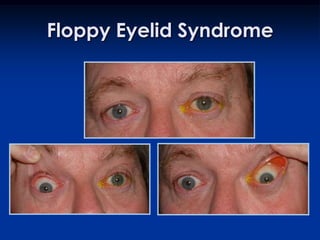
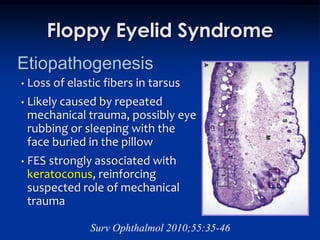
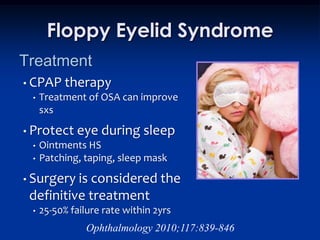
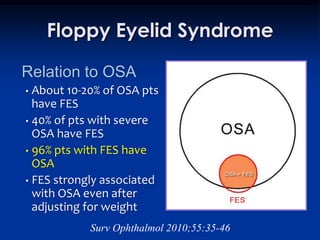
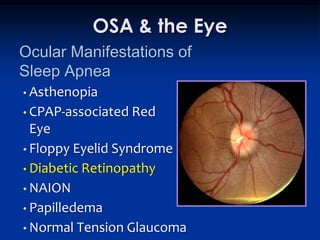
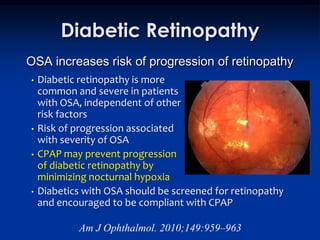
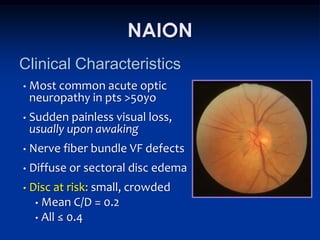
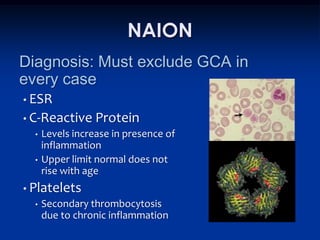
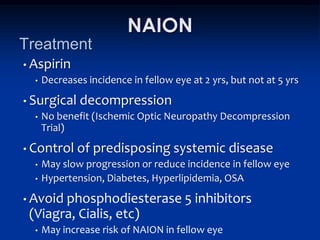
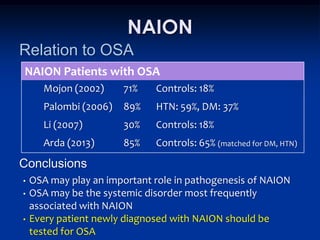
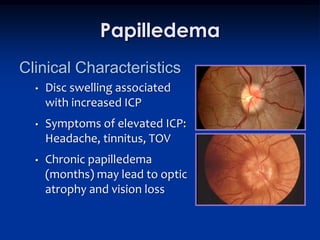
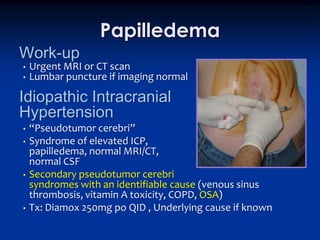
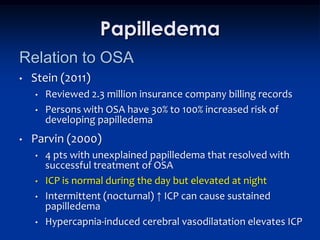
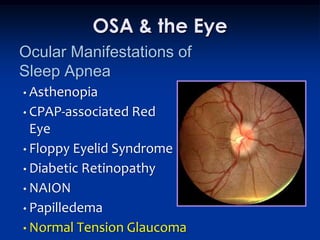
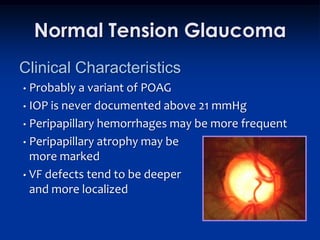
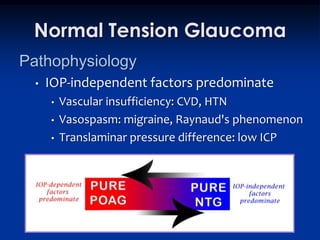
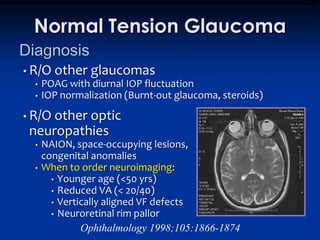
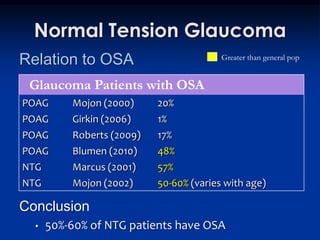
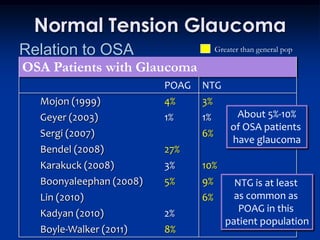
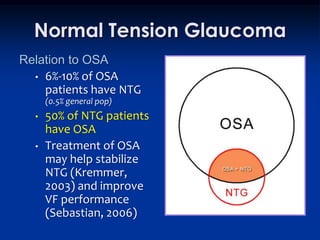
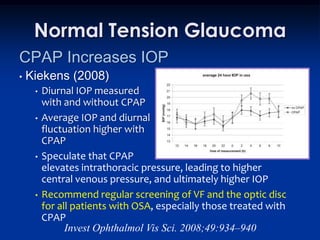
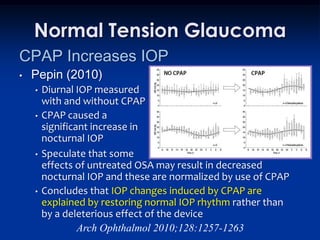
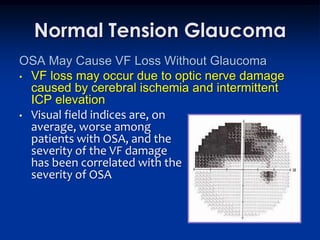
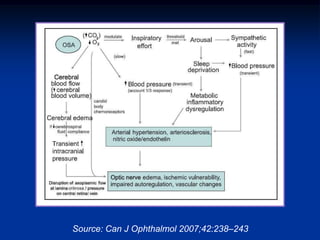
This document discusses sleep apnea and its ocular manifestations. It begins by defining sleep apnea and describing how it is diagnosed and treated. It then outlines several ocular conditions that are associated with sleep apnea, including asthenopia, CPAP-associated red eye, floppy eyelid syndrome, diabetic retinopathy, non-arteritic anterior ischemic optic neuropathy (NAION), papilledema, and normal tension glaucoma. For each condition, it discusses the clinical characteristics, pathogenesis, and relationship to sleep apnea. It emphasizes that screening for and treatment of sleep apnea can help prevent or improve some of these ocular conditions.