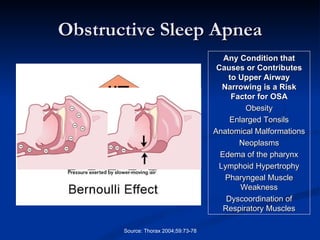
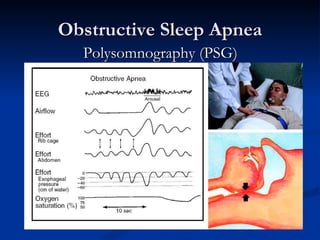
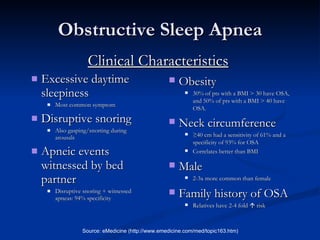
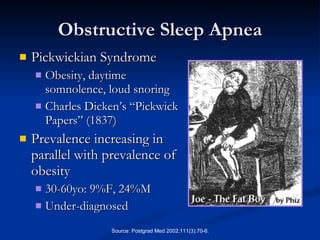
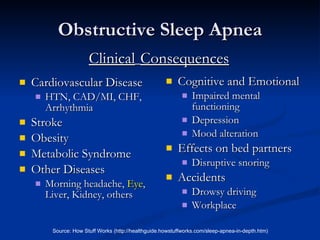
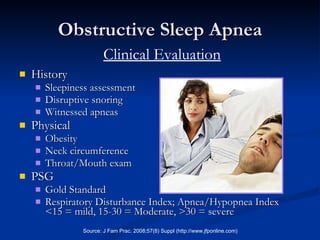
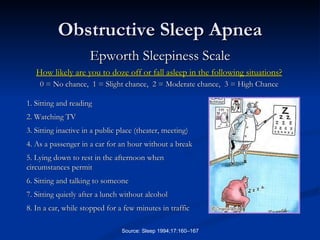
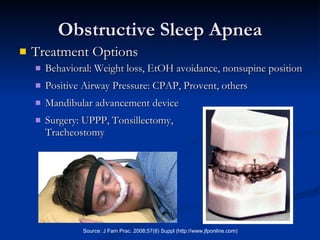
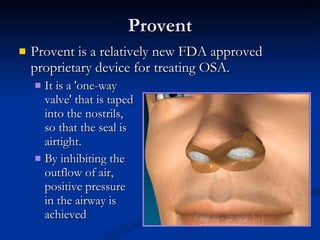
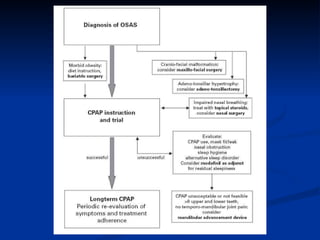
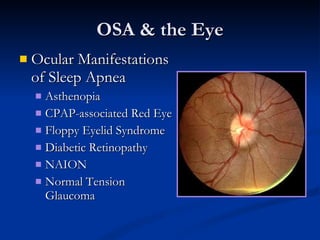
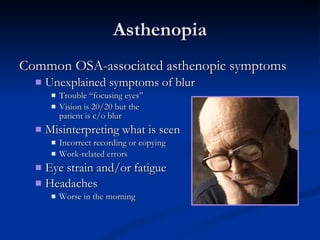
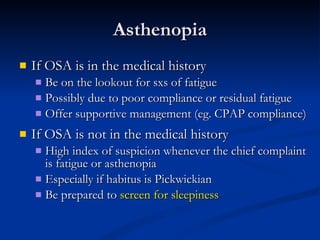
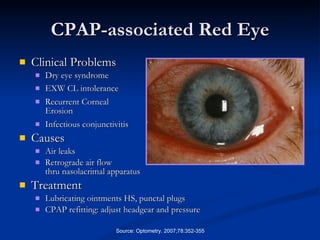
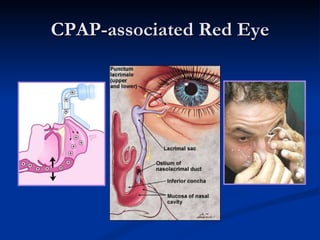
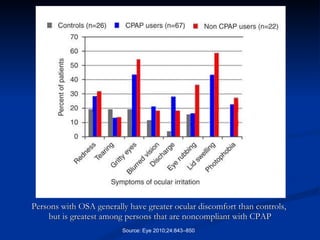
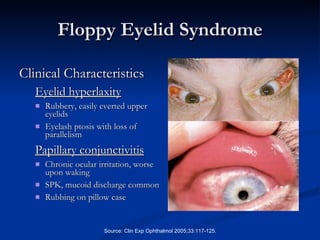
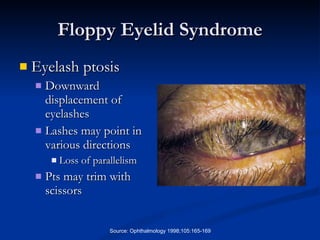
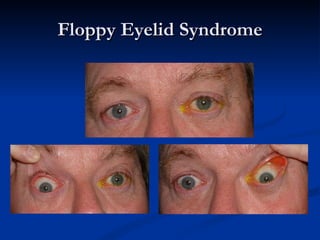
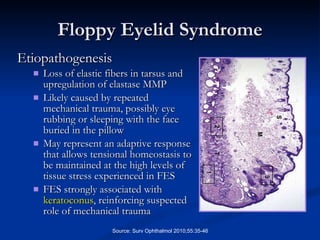
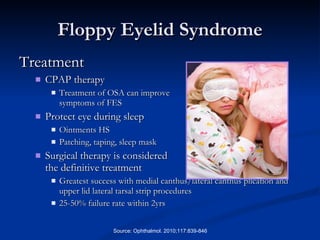
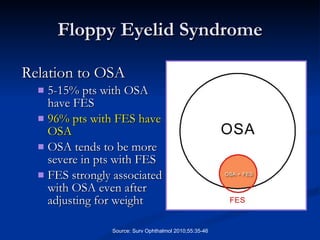
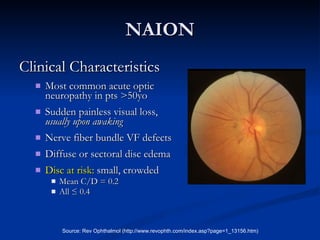
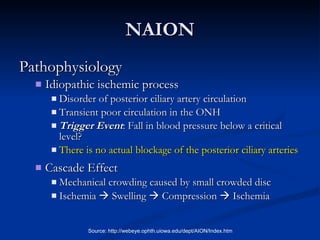
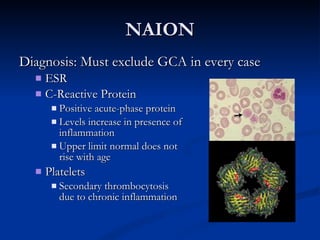
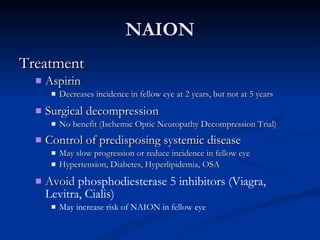
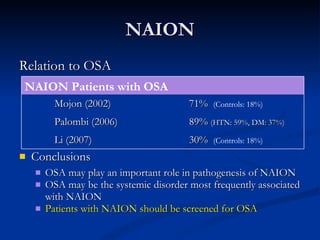
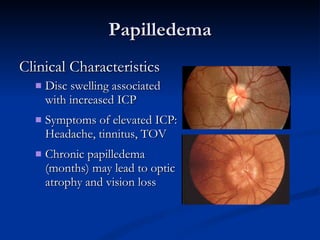
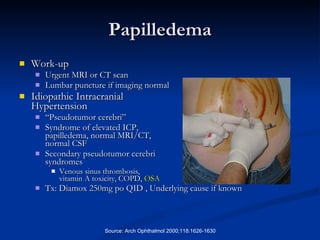
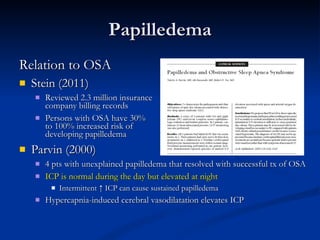
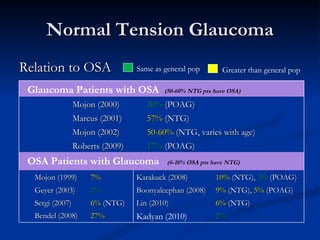
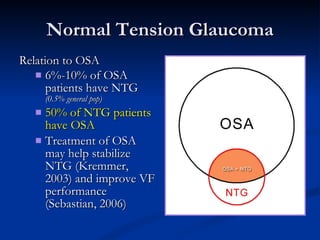
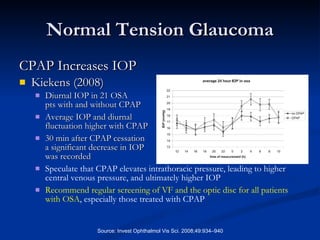
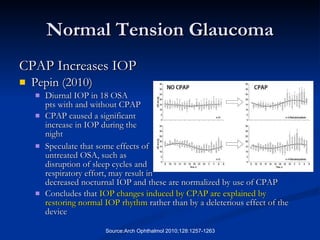
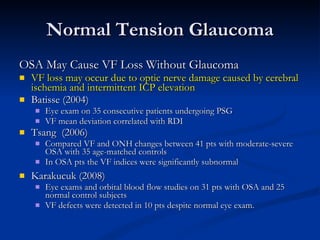
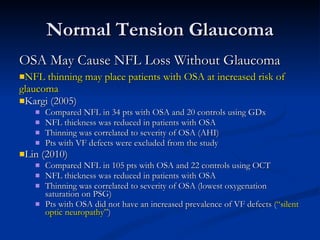
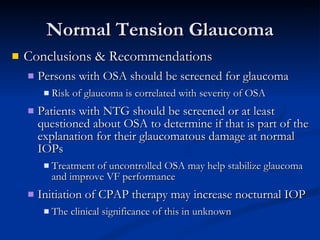
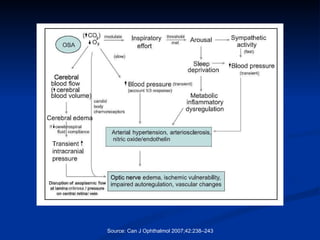
The document discusses sleep apnea and its ocular manifestations. It describes obstructive sleep apnea, including risk factors, clinical signs and symptoms, diagnosis using polysomnography, and treatment options like CPAP. It then summarizes several ocular conditions associated with sleep apnea, such as asthenopia, CPAP-associated red eye, floppy eyelid syndrome, increased risk of diabetic retinopathy progression, non-arteritic anterior ischemic optic neuropathy, and papilledema. Screening sleep apnea patients for these eye conditions and encouraging CPAP compliance can help prevent or slow their progression.
![Sleep Apnea & the Eye Rick Trevino, OD Rosenberg School of Optometry University of the Incarnate Word [email_address]](https://image.slidesharecdn.com/osa2011-110913223640-phpapp01/85/Sleep-Apnea-The-Eye-2011-1-320.jpg)