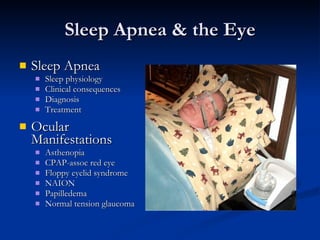
The document summarizes sleep apnea and its ocular manifestations. Obese middle-aged men with sleep apnea often experience excessive daytime sleepiness, disruptive snoring, and witnessed apneas during sleep. Common ocular manifestations of sleep apnea include asthenopia, CPAP-associated red eye, floppy eyelid syndrome, non-arteritic anterior ischemic optic neuropathy (NAION), papilledema, and normal tension glaucoma. Sleep apnea has been linked to an increased risk of developing these eye conditions.
![Sleep Apnea & the Eye Rick Trevino, OD VA Outpatient Clinic Evansville, IN [email_address]](https://image.slidesharecdn.com/sleep-apnea-and-the-eye-2008-8733/85/Sleep-Apnea-and-the-Eye-2008-1-320.jpg)